Acute Myocardial Infarction Associated with Severe Fatal Ulcerative Colitis-Juniper Publishers
Abstract
A case of acute myocardial infarction (MI) in a young woman presenting with first episode of ulcerative colitis (UC) is presented. The patient had a rapidly deteriorating clinical course with a fatal outcome. The cardiac manifestations of ulcerative colitis and its association with myocardial infarction is discussed.
Introduction
Inflammatory bowel diseases (IBD) include Ulcerative colitis (UC) and Crohn’s disease (CD). Both the conditions may present with a variety of extra-intestinal manifestations. Myocarditis and pericarditis are the most common cardiac manifestations of ulcerative colitis (UC). UC also predisposes to arterial and venous thromboembolic complications. A few cases of myocardial infarction (MI) in association with UC have been reported. However, the association between UC and MI is uncertain. We report a case of acute MI in a young female presenting with first episode of UC. The patient succumbed to her illness due to the uncontrolled disease activity. Cardiac complications might be reflective of the severity of UC and active surveillance for the same is warranted, in patients with UC.
Case Report
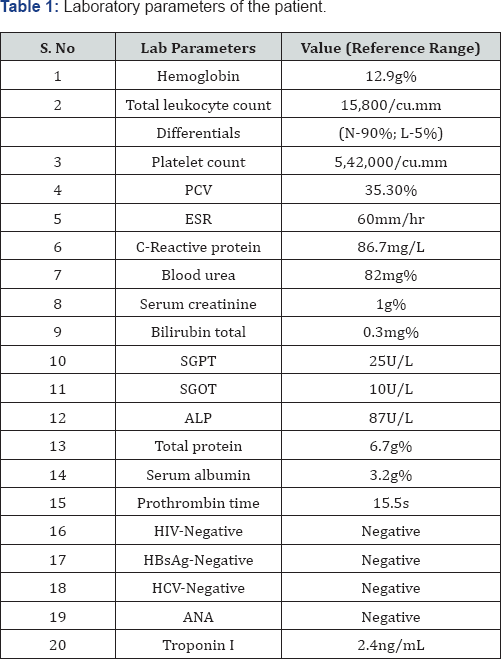
A 18 year old female presented with symptoms of diffuse abdominal pain for a duration of 3 weeks, followed by bleeding per rectum (PR) for 2 weeks. The abdominal pain was associated with an urge to defecate. There were no specific pain aggravating or relieving factors. She reported that her stools were semisolid and mixed with blood with intermittent episodes of frank bleeding PR. She denied symptoms of vomiting, fever or any prior medications. On examination, the patient was afebrile, mildly pale. Her blood pressure was 100/80mmHg, pulse rate of 98/ min and an oxygen saturation of 99% while breathing room air. There was diffuse tenderness on abdominal palpation and there was no organomegaly. The patient was admitted to the emergency department and the initial evaluation (Table 1) was supportive of an inflammatory bowel disease (IBD). The patient underwent colposcopy the next day and was found to have loss of vascular pattern and evidence of granularity, friability and multiple ulcers in the descending colon, sigmoid colon and rectum. Histopathologic examination confirmed the diagnosis of UC. On day 2 of hospitalization, the patient complained of persistent chest pain. An electrocardiogram (ECG) was done and it revealed ST elevation in limb leads II, III, aVF (Figure 1). Serum troponin levels done six hours later were elevated. Echocardiography showed wall motion abnormality involving the mid inferior and inferoseptal septal regions. The patient was diagnosed to have inferior wall MI and was transferred to coronary unit. She was initiated on clopidogrel, atorvastatin and heparin. Following a transient improvement, her clinical status deteriorated with multiple episodes of bloody diarrhea compromising her hemodynamic status. Her symptoms remained refractory to intravenous (iv) steroids and mesalamine enema. Despite intensive resuscitation with fluids, intravenous inotropes, blood transfusion, hypokalemia correction, the patient succumbed to her illness. A coronary angiogram (CAG) could not be done due to her refractory diarrhea causing hemodynamic instability.
a) Stool microscopy: No ova/cyst; 40-60 leukocytes/hpf; numerous RBCs/hpf; no abnormal deposits; no growth on culture
b) Chest X-ray: Normal cardiothoracic ratio; no evidence of gross pleural/pericardial effusion
c) X-ray abdomen: No air fluid level; no air under diaphragm
d) USG abdomen: Thickened descending and transverse colon. Small bowel loops thickened with average thickness 6.5mm. Gall bladder distended. Liver, spleen, pancreas normal.
Discussion
Several systemic chronic inflammatory diseases, especially rheumatoid arthritis, systemic lupus erythematosus have been found to be associated with an increased risk of ischemic heart disease, after adjustment for known cardiac risk factors. Both UC and Crohn's disease (CD) may present with a variety of cardiac manifestations. The most common cardiovascular complication in IBD is pericarditis [1]. The various causes of pericardial involvement in IBD include drugs (5-ASA, etc), pericardio- colonic fistulas or can be idiopathic [2] and it may occasionally be the presenting symptom. IBD can also lead to endocardial or myocardial involvement. Endocarditis and subendocardial abscess can occur secondary to septicemia and immunosuppression. Exacerbations of IBD may be manifested with myocarditis. Autoimmunity has been proposed as the pathogenetic mechanism in such cases. Myocarditis can also be seen as a side-effect of medications such as 5-aminosalicylic acid (5-ASA). Compared to Crohn's disease, patients with UC may be at a higher risk for myocarditis. Selenium deficiency during total parenteral nutrition, prolonged use of steroids are also likely to contribute to cardiac involvement in IBD. Cardiac involvement occasionally may result in heart failure. Various causes of acute heart failure in IBD include acute MI, myocarditis, cardiac tamponade and valve deterioration due to endocarditis. Valvular and myocardial involvement are the usual causes of chronic heart failure. Another important cause of cardiac involvement is secondary to steroid use. There have been few reported cases of heart muscle atrophy during prolonged use of corticosteroid [3].
IBD patients are also at an increased risk for both arterial and venous thromboembolism [4] and are among the leading causes of death in UC. The risk for thromboembolism appears to be multifactorial and may be related to mucosal inflammatory activity. However, the involvement of coronary arteries in UC is rare. Such complications usually occur during the acute phase of the disease [5]. Reports of AMI in UC are scarce [6,7]. The causal relationship between UC and MI is not established. In almost all of the reported cases, MI occurred during relapse or exacerbation of UC. The pathogenesis might involve a surge of inflammatory mediators, raised levels of coagulation factors [8], antiphospholipid antibodies [9] observed during active disease. These mediators might favor a thrombotic milieau culminating in MI. MI causes heart related sudden death in UC. In a study, 2 out of 1407 operated UC patients died of myocardial infarction [10]. However, with regard to the cardiovascular risk factors, IBD patients do not seem to be different from the general population, except for cholesterol levels. Studies in hospitalized or malnourished IBD patients showed significantly lower cholesterol levels [11]. Some studies [12] have reported an increased risk of cardiac events in IBD patients. However, a recent retrospective cohort study found no difference in the incidence of acute coronary syndrome, after adjustment for known cardiac risk factors, compared to general population [13]. A more recent population-based study that examined a combined end point of ischemic heart disease and reported a slightly increased risk in patients with UC and CD [14]. However, the study did not adjust for known cardiac risk factors. As emphasized earlier, cardiovascular complications may also occur during treatment with high dose steroids [7] or other immunosuppressants. To our knowledge, this is the first reported case where the first episode of UC, before treatment initiation, is complicated by MI. Our patient exhibited an intense inflammatory burden, as evidenced by the increased inflammatory markers. Although it can be derived that coronary complications are more likely in patients with severe disease, lack of adequate data hinders a systematic analysis. A similar case of MI in UC complicated by cardiac arrest has been reported [15], where the patient developed MI following steroid treatment. In our patient, the mortality was more due to the bowel disease severity than the cardiac complication per se.
Conclusion
Patients diagnosed with UC should be actively monitored for cardiovascular complications, particularly at times of relapse or exacerbations. Cardiovascular complications might be present at the onset of the disease and might be reflective of the severity of the disease and warrant intensive management.
For more Open Access Journals in Juniper Publishers
please click on: https://juniperpublishers.com/open-access.php
For more articles in Open Access Journal of Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment