Undetected pulmonary Artery Aneurysms Secondary to Prolonged Right-sided Endocarditis in a Patient with Corrected Tetralogy of Fallot-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Mycotic pulmonary artery aneurysms are a rare
complication of right-sided endocarditis most often associated with
congenital heart disease or intravenous drug addiction. We report a case
of undetected mycotic pulmonary artery aneurysms secondary to prolonged
right-sided endocarditis in a 25-years old patient with corrected
tetralogy of Fallot /pulmonary atresia. An attempt to explain the
delayed diagnosis of endocarditis with subsequent mycotic aneurysms
formation is made and the clinical and imaging findings of this rare
complication during a long-term follow up are presented, contributing to
our knowledge on the natural history of this disease.
Keywords: Mycotic aneurysms; Tetralogy of Fallot /pulmonary atresia; Right heart endocarditis; Kocuria varians
Abbreviations: CT: Computed
Tomography; TTE: Trans Thoracic Echocardiogram; MRI: Magnetic Resonance
Imaging; MRA: Magnetic Resonance Angiography; PAAs: Pulmonary Artery
Aneurysms
A 25-years old man, with corrected tetralogy of Fallot/
pulmonary atresia at the age of 5 years and subsequent
angioplasty for pulmonary artery conduit stenosis at the age of
20 years, presented with hemoptysis, low grade fever, signs of
right heart failure and splenomegaly. During last five years and
shortly after the conduit angioplasty he also referred multiple
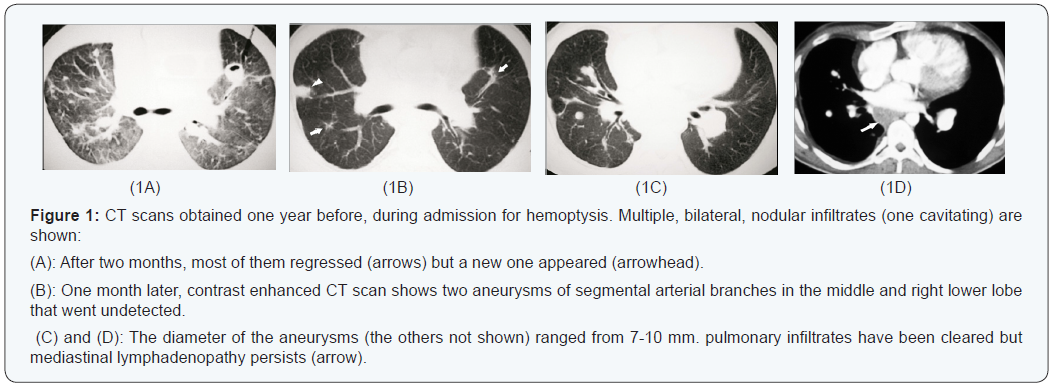
episodes of hemoptysis. In-hospital serial chest computed
tomography (CT) scans during each admission (Figure 1) showed
multiple migrating infiltrates and nodules and mediastinal
lymph adenopathy with only temporary regression after short
term antibiotic therapy. Considering retrospectively previous
chest CT scans, we noticed the presence of multiple, bilateral
pulmonary artery aneurysms (PAAs), unchanged in number and
size (7-10mm in diameter) for the last two years before current
admission (Figure 1). The aneurysms were not apparent on the
initial evaluation (but contrast enhanced studies were missing
at that time). Additionally, despite the broad diagnostic workup
performed in each admission time, which also included cardiac
echocardiography, cardiac magnetic resonance imaging (MRI)
and bronchoscopy, the cause of hemoptysis remained unclear.
The patient underwent a chest high resolution CT scan
(not shown) revealing patchy infiltrates and a trans thoracic
echocardiogram (TTE). The pulmonary valve was highly
echogenic with significant stenosis and regurgitation indicating
major degeneration. Furthermore, from the supra sternal view
an oscillating nodular mass attached inside the conduit was
demonstrated indicating possible vegetation or thrombus
(Figure 2). However, a high index of suspicion for endocarditis
was justified since the mass was attached in the physically
damaged endothelium by the high turbulent flow of the stenotic
right ventricular outflow tract. Trans esophageal echo was
not performed since it could not give significant additional
information.

Blood cultures were taken and intravenous antibiotic
treatment for endocarditis was initiated with vancomycin and gentamycin and then with penicillin G after the detection
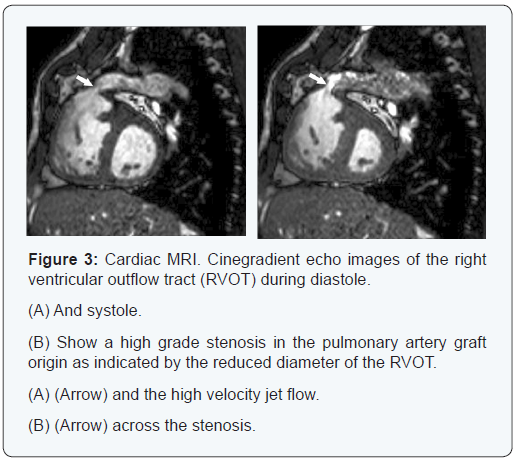
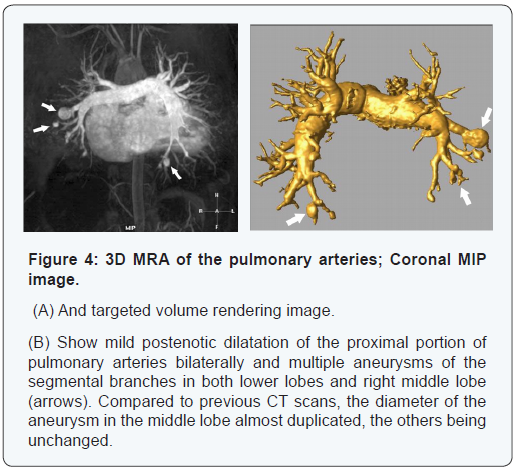
of Kocuria Varians. Cardiac MRI and magnetic resonance
angiography (MRA) of the pulmonary vessels revealed graft
conduit stenosis, pulmonary valve regurgitation, impaired right
ventricular function and multiple aneurysms located in the
pulmonary artery segmental branches of both lower lobes and
right middle lobe (Figures 3 & 4). Since last CT evaluation (one
year before), the aneurysms remained unchanged in number
and size except for the one in the middle lobe which was found
to have been almost duplicated.
The diagnosis of multiple mycotic PAAs due to endocarditis
was confirmed. Hemoptysis ceased shortly after hospital
admission and therefore, it was attributed to septic pulmonary
embolism, as it was presumably the case in his previous
admissions. Aggressive surgical or interventional management for the PAAs had not been recommended. A new echocardiogram
after 30 days administration of the appropriate antibiotic
treatment did not show the vegetation of the conduit. The
treatment was discontinued and the patient was discharged
afebrile. A surgical replacement of the valvular graft was
successfully performed one month later. The patient had a
straightforward course but he refused a repeat CT scan.
Mycotic PAAs are most commonly seen after right heart
endocarditis often associated with congenital heart disease
or IV drug use and their detection needs a high index of
suspicion in the appropriate clinical setting. Detection of
large PAAs is straightforward even with conventional chest
CT after i.v contrast administration, [1] but small PAAs need
the application of dedicated angiographic techniques using
either multi slice CT or MRI. Angiography, however, is felt to
be the best diagnostic procedure and can be combined with
percutaneous catheter embolization [2] Bronchoscopy and/or
inadvertent biopsy of a PAA can lead to massive hemorrhage
and death [2]. Owing to their rarity, their natural history is not
well documented. It is reported that about one-third of PAAs
rupture, causing death but the relationship between size and
location of PAAs and their risk of rupture is not known [1]. In
a series of cases, more than 50% of patients have been shown
to die as a result of bleeding complications [3] and the need for
urgent treatment is established. Treatment for PAAS is directed
towards the underlying etiology and can be conservative or
invasive. Regression under conservative treatment has been
scarcely reported [1]. Definitive therapy involves surgical or
endovascular approaches.
For more articles in Open Access Journal of Cardiology & Cardiovascular
Therapy please
click on:
https://juniperpublishers.com/jocct/index.php
https://juniperpublishers.com/jocct/index.php


Comments
Post a Comment