Successful Percutaneous Intervention for Chronic Total Occlusion of Left Subclavian Artery-Juniper Publishers
Abstract
Introduction: Subclavian artery stenosis is most commonly caused by atherosclerotic disease. Surgical treatment is associated with high morbidity and mortality. Intervention is generally reserved for the management of symptomatic patients who present with upper limb ischemia, Vertebrobasilar symptoms and subclavian steal syndrome. Endovascular stenting is preferred over surgery because of high success rate, less invasive and minimal complications.
Case report: Here we report a case of 56 year old female patient with history of hypertension and diabetes presented with dizziness, vertigo and left arm claudication with use of her left upper extremity since last six months. She was diagnosed as a case of subclavian steal syndrome.
Treatment: Patient underwent successful Percutaneous Transluminal Angioplasty (PTA) of the left subclavian artery with marked improvement of symptoms at follow-up. Patient was monitored with Duplex ultrasound of left subclavian artery, measurement of BP and examination of pulse at each visit.
Conclusion: PTA is an effective with high success rate, less invasive and minimal complications when compared to surgery for the treatment of symptomatic subclavian artery stenosis. However, regular clinical and Duplex ultrasound assessment of subclavian artery is necessary after angioplasty for monitoring restenosis.
Keywords: Subclavian steal syndrome (SSS); Percutaneous transluminal angioplasty (PTA); Subclavian artery stenosis; Intervention; Atherosclerotic disease
Introduction
Subclavian artery stenosis is most commonly caused by atherosclerotic disease. Stenosis typically occurs in the first part of the subclavian artery proximal to the origin of the vertebral artery extending from the ostium to the origin of the vertebral artery. The incidence of left subclavian artery stenosis is far higher than that of right subclavian artery stenosis.
Intervention is generally reserved for the management of symptomatic patients who present with upper limb ischemia, Vertebrobasilar symptoms and subclavian steal syndrome. Endovascular stenting is preferred over surgery because of high success rate, less invasive and minimal complications. Here we report a case of 56 year old female patient presented with subclavian steal syndrome whom we successfully treated with percutaneous transluminal angioplasty (PTA).
Case Report
A 56 year old female patient with history of hypertension and diabetes presented with dizziness, vertigo and left arm claudication with use of her left upper extremity since last six months.
On physical examination
Inability to measure BP on left arm with absent left radial pulse and right upper limb BP was 160/80mmHg. There were no signs of ischemia in left upper extremity.
Investigations
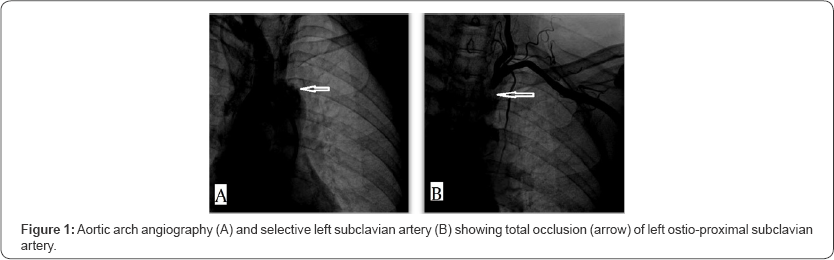
Electrocardiogram showed sinus rhythm with no ST-T changes, Transthoracic echocardiography revealed good biventricular function with type 1 diastolic dysfunction. Coronary angiography selective left subclavian angiography revealed total occlusion of showed mild single vessel disease. Aortic arch angiography and left ostio-proximal subclavian artery (Figure 1).
Procedure
The procedure was performed under local anaesthesia. The right femoral artery and left brachial artery were accessed percutaneously with 8F and 6F introducer sheaths, respectively A preprocedural loading dose of Aspirin 325mg and 600mg of clopidogrel was given. Intravenous heparin 100IU/kg and antibiotic were given.
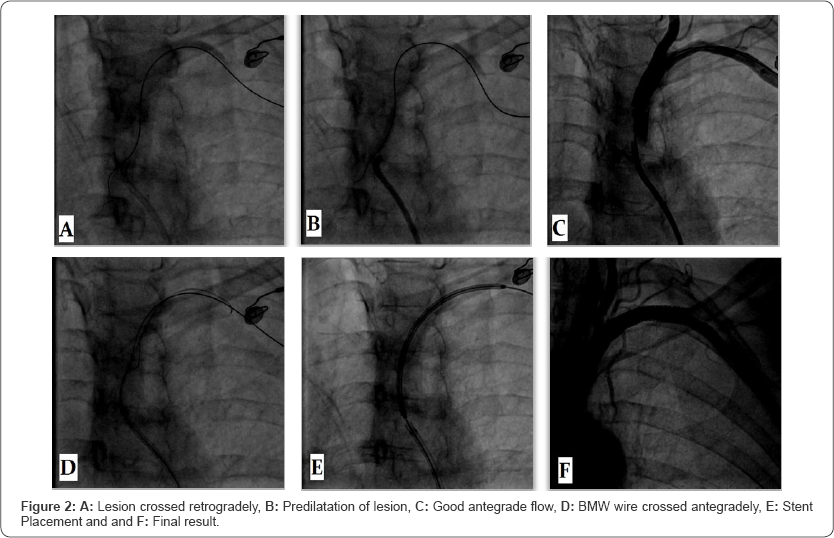
Ostia of left subclavian artery was engaged by using JR 7F guiding catheter. Check angio showed total occlusion. A 6F shuttle sheath was used to cannulate the vessel and placed distal to the occlusion. The lesion was crossed retrogradely using 0.014x190cm cross-it 200 and placed in proximal descending aorta (Figure 2A). Lesion was predilated using 3.5x15mm balloon at 8atm pressure (Figure 2B). Check angiogram through JR guiding catheter established good antegrade flow with no dissection (Figure 2C). Using another 0.014x180cm BMW wire crossed the lesion antegradely and the cross-it 200 wire removed (Figure 2D). An 8x32mm INVATEC scuba stent was deployed across ostio- proximal subclavian artery (Figure 2E) with a good angiographic result (Figure 2F).
Post procedure course was uneventful. The patient was discharged after three days with Aspirin 150mg OD, Clopidogrel 75mg BD and Rosuvastatin 40mg OD.
Follow-up
Patient was followed up at 1, 3, 6 months and one year. Patient reported marked improvement of symptoms. At each visit, patient was monitored with Duplex ultrasound of left subclavian artery, measurement of BP and examination of pulse.
Discussion
Atherosclerosis is the most common cause of subclavian stenosis and, thus, steal syndromes, irrespective of the clinical manifestation [1-3]. However, other causes include large artery vasculitis, thoracic outlet syndrome, and stenosis after surgical repair of coarctation of aorta or tetralogy of Fallot.
The presence of subclavian stenosis is associated with increased total mortality (hazard ratio, 1.40) and cardiovascular disease mortality (hazard ratio, 1.57) [2] and with an increased risk of cerebrovascular ischemic events related to progressive carotid stenosis and compromised collateral pathways. Thus, subclavian artery stenosis is a cardiovascular risk marker and require aggressive secondary prevention.
Even asymptomatic subclavian artery stenosis is associated with increased risk of morbidity and mortality related to underlying atherosclerotic disease burden in other vascular beds [2-4]. Symptomatic patients with proximal subclavian artery occlusive disease can be successfully treated either surgically or percutaneously [5-12].
First case report of subclavian angioplasty was done by Bachman & Kim [13]. After this report, percutaneous intervention of subclavian disease has grown persistently, becoming the mainstay of therapy. Balloon angioplasty and stenting can be performed when stenting is unlikely to compromise the vertebral circulation. Technical success of the percutaneous approach can be achieved in >90%, with 5-year patency rates of 85% [12]. Complications during subclavian artery intervention are stroke (<1%), dissection, access site complications (0-5%) like hematoma formation, thrombosis and pseudoaneurysm formation.
The major long-term risk of subclavian artery intervention is restenosis. Stenting appears to have significantly reduced the rate of restenosis, from 15-20% with angioplasty to 0-10%. The treatment for restenosis will depend on its etiology. Failure to cover the ostium or Inadequate stent expansion may be treated with repeat angioplasty and, sometimes, re-stenting. Alternatively, surgical revascularization using an extrathoracic approach (carotid-subclavian, axillo-axillary) is a reasonable option in a symptomatic patient who is an operative candidate.
Conclusion
PTA is an effective with high success rate, less invasive and minimal complications when compared to surgery for the treatment of symptomatic subclavian artery stenosis. However, regular clinical and duplex ultrasound assessment of subclavian artery is necessary after angioplasty for monitoring restenosis.
Conflict of Interest
The author(s) declare(s) that there is no conflict of interest regarding the publication of this paper.
Informed Consent
Written informed consent was obtained from patient for publication of this case report and accompanying images.
For more Open Access Journals in Juniper Publishers
please click on: https://juniperpublishers.com/open-access.php
For more articles in Open Access Journal of Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment