Micro-Bubbles in the Left Heart-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
The information provided by diagnostic imaging technologies is an invaluable tool for managing cardiology patients. However, one must be careful not to make clinical decisions based exclusively on an image produced by diagnostic devices because; occasionally this approach could prove misleading. Micro-bubbles in the left heart in a patient undergone mitral valve replacement (MVR) three years back are uncommon and require further evaluation. The differential diagnosis being paradoxical air embolism through a PFO, left atrial rupture, atrial-bronchial or atrial-esophageal fistula and Cavitations/De-gassing. The Cavitation/De-gassing phenomenon is caused by the local pressure drop that occurs during the closure and/or opening of mechanical valve leaflets. Occasionally, these peculiar features of echo cardiographic images generated by cavitations can simulate a mass or vegetation and are a potential source of diagnostic error. A clinical case that illustrates this phenomenon is described.
Keywords: Cavitation; Mechanical valve; Vegetation; Micro-bubbles
Introduction
The information provided by echocardiography is an invaluable tool for managing cardiology patients. However, one must be careful not to make clinical decisions based exclusively on echocardiography image interpretation because; occasionally this approach could prove misleading. We describe a case thathad undergone mitral valve replacement (MVR) three years back presenting with fever and chills. Blood culture showed no growth. Screening 2D trans-thoracic echo (TTE) showed hyperechoic micro-bubbles in the left atrium and left ventricle. The origin of these micro-bubbles was a diagnostic dilemma.
Case Report
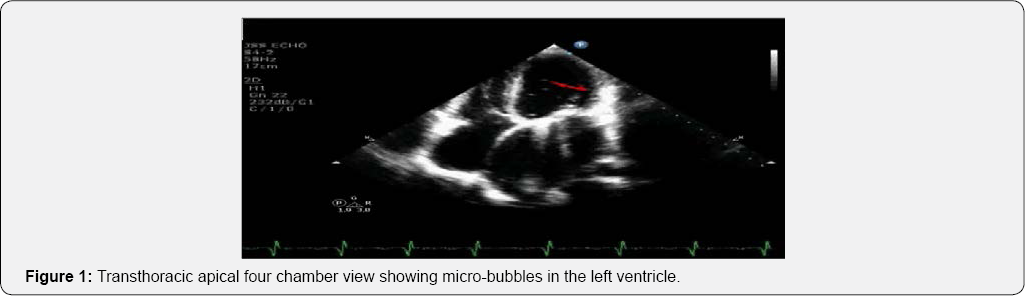
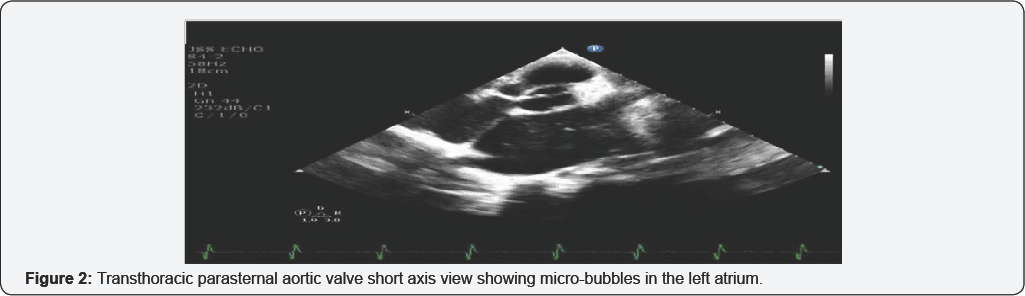

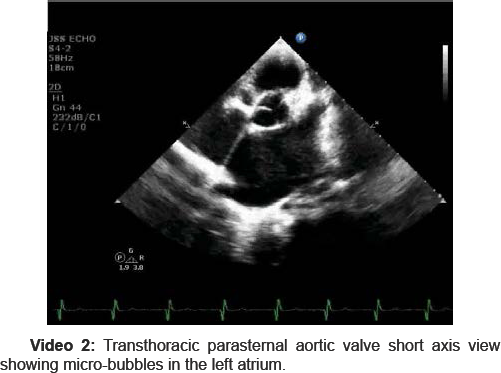
A 25 year old male patient presented with fever associated with chills of one week duration. He was evaluated by a physician for fever and all the diagnostic evaluation was negative. Blood culture did not show any growth. He was referred to us for echo screening to rule out culture negative Infective endocarditis. TTE showed dilated left atrium, normal prosthetic valve function with washing jets, mean gradient of 9mm of Hg, good bi-ventricular function. But there were hyper-echoic micro-bubbles in the left atrium and left ventricles (Figure 1 & 2 and Video 1 & 2). They probably arose near the mechanical valve and were seen both in the left atrium and left ventricle. These microbubbles were not seen in left ventricular outflow tract and the aorta. He had undergone MVR (TTK Chitra heart valve 27mm) three years back when he was diagnosed to have rheumatic heart disease with severe calcific mitral valve stenosis in sinus rhythm and good bi-ventricular function. Following replacement intra-operative transoesophageal echocardiography and postoperative TTE screening showed normal prosthetic valve function with washing jets, mild pulmonary hypertension with good bi-ventricular function. No clots, vegetation or pericardial effusion. The microbubbles were not seen in these echo cardio-graphic evaluations.
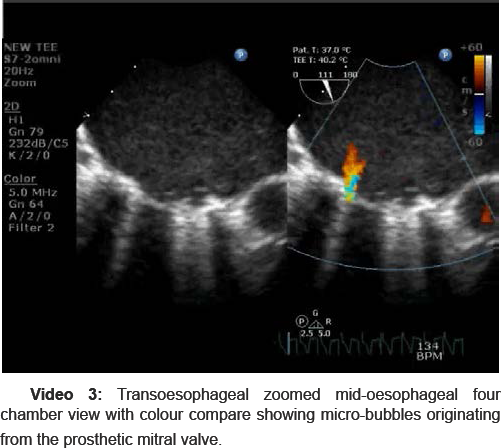
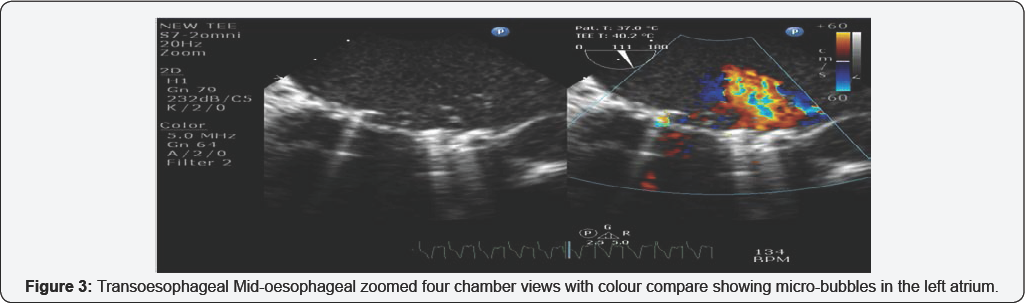
Careful evaluation of the images showed that micro-bubbles were arising from the prosthetic valve, when the occluderis closing against the sewing ring. There was no pericardial effusion which ruled out left atrial rupture. CT scan did not revel any fistula between the left atrium and bronchus or oesophagus. TEE also showed that micro-bubbles were seen in the left atrium and left ventricle (Figure 3 and Video 3). Normal prosthetic valve function. No pannus or vegetation. Mean gradient across mitral valve was 9mm of Hg. Good bi-ventricular function.
Discussion
The TTK Chitra mechanical valve is a tilting disc valve developed in India. The valve has an integrally machined cobalt- based alloy cage, an ultra-high molecular-weight polyethylene disc, and a polyester suture ring. An important feature of this valve is its soft closing sound, by virtue of a plastic occlude [1]. Microbubbles in the left heart can be due to cavitation or degassing, paradoxical air embolism through an atrial septal defect (ASD) or PFO, left atrial to bronchus or oesophageal fistula and inadequate deairing following an open heart procedure. Left atrial to bronchial or oesophageal fistula are seen most commonly following radiofrequency ablation for atrial fibrillation [2,3].
Micro-bubbles noted in the left heart following native valve replacement have been attributed to mechanical heart valves, predominately in the mitral position [4,5]. These micro-bubbles have not been reported to occur with bio-prosthetic valves. Cavitation, is vaporization of blood by a localized rapid pressure drop at the site of closure of the prosthetic valve occluder and sewing ring [6,7]. These gas bubbles formed redissolve in normal pressures of the cardiac chambers. They usually do not reflect any mitral prosthetic valve abnormality. Cavitation was first directly associated with mechanical heart valves in the mid-1980s after a series of valve failures noted with the Edwards-Duromedics valve (Edwards Laboratories, USA) [8]. The observed damages indicated that cavitation may have been responsible. It is an erosive phenomenon that occurs during mechanical heart valve closure when the local pressure drops below vapor pressure. The formation of stable gas bubbles may result in gaseous emboli and secondarily cause transient ischemic attacks or strokes [9]. Cavitation may also cause erosion of prosthetic heart valve material; consequently, this phenomenon has been claimed to be partly responsible for the increased risk of haemolysis and fatal valve failure seen in patients with prosthetic heart valve [10]. Cavitation has been extensively studied in vitro; however, in vivo studies examining this effect are scarce. All of these studies confirm that cavitation potential is exclusive to mechanical heart valves and that gas bubble formation is not observed in bioprosthetic or native valves. All mechanical valves investigated show cavitation under different conditions. Griod G et al has studied in an in vitro model using the water circuit system enriched with carbon dioxide (CO2) passing through a Venturi tube. They concluded that cavitation is transient phenomenal (several milliseconds) and happens under a higher pressure gradient. The degassing (Vaporization of CO2) produces micro-bubbles lasting up to as long as more than one second under much lower pressure. This in vitro study suggests that micro-bubbles observed during several hundred milliseconds after the opening of prosthetic cardiac valves are the result of degassing of CO2 in blood rather than a cavitation phenomenon as suggested in the literature [4]. The transesophageal echocardiography approach is the best method for assessing artificial heart valves. Physicians managing patients with prosthetic valves should be familiar with the characteristics of normal and abnormal functioning prosthetic valves. They should be able to recognize the spontaneous echo contrast, microbubbles, strands, sutures, vegetations and thrombi [11].
Conclusion
Echo cardiographers must be aware of the cavitation and degassing phenomenon. The gaseous micro-bubbles formation is seen with mechanical valves only and more common in the mitral position. They usually do not reflect any mitral prosthetic valve abnormality. Micro-bubbles in the left heart can be due to inadequate deairing following an open heart procedure, cavitation or degassing, paradoxical air embolism through the atrial septal defect, left atrial rupture or a fistula between the left atrium and bronchus or oesophagus. Occasionally it maybe misdiagnosed as vegetation or mass attached to mechanical valve. In our case alteration in the viscosity of blood secondary to fever and dehydration probably predisposed for the development of micro-bubbles in the left heart, as it was not seen in the previous echo cardio-graphic examination.
For more Open Access Journals in Juniper Publishers
please click on: https://juniperpublishers.com/open-access.php
For more articles in Open Access Journal of Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment