A Review on Coronary Bioresorbable Vascular Scaffold System-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Historically biodegradable materials for implants which serve as a temporary function have been used in therapeutic medicine in areas that includes wound closure, interventional technologies, drug delivery, oncology and cardiovascular surgery and were designed to overcome the disadvantages of permanent metallic based devices. Various types of materials are used for the development of scaffold strut like polymers (poly-L-Lactic acid, tyrosine poly carbonate) and alloys (Mg, platinum). BVS (bioresorbable vascular scaffold) are mainly useful for the restoration of functional endothelial coverage, allows the restoration of physiological vasomotion, allow to graft stented segments of coronary artery, enables prevention of acute recoil or occlusion, provide inhibition of in segment restenosis through efficient drug elusion and no foreign material left behind. Along with the advantages there are some disadvantages like higher target lesion revascularization rates compared with Drug Eluting Stents (DES).
Keywords: BVS; CAD; Restenosis; Revascularization; Intervention technology
Introduction
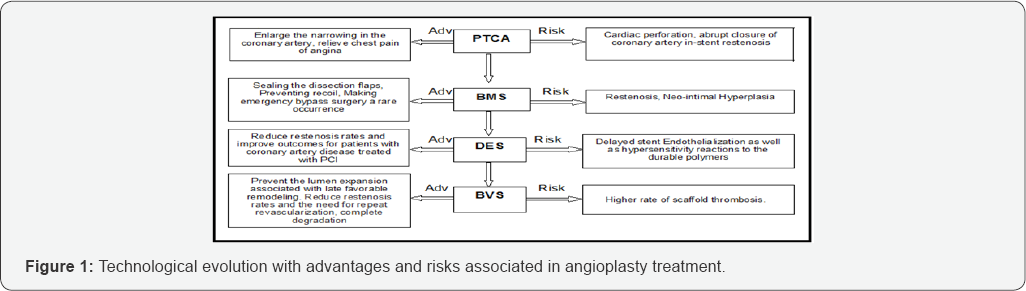
Coronary Artery Disease (CAD) is the most common type of heart disease. It is the leading cause of death. CAD happens when the arteries that supply blood to heart muscle become hardened and narrowed. This is due to the buildup of cholesterol and other material, called plaque on their inner walls. As it grows, less blood can flow through the arteries. As a result, the heart muscle can’t get the blood or oxygen it needs. Over time, CAD can also weaken the heart muscle and contribute to heart failure and arrhythmias. Heart failure means the heart can’t pump blood well to the rest of the body. Arrhythmias are changes in the normal beating rhythm of the heart [1]. CAD treated by surgery and other procedures includes balloon angioplasty, stent placement and coronary artery bypass surgery [2]. Percutaneous transluminal coronary angioplasty (PTCA) is a minimally invasive procedure used to open blocked coronary arteries to improve blood flow and allow blood to circulate to the heart muscle. Using a balloon to dilate a stenotic vessel usually results in a small dissection in the vessel wall. Prior to the introduction of stent technology, larger dissection often resulted in the patient requiring emergency bypass surgery, whereas stents can now be used to support the vessel wall from the inside. This re-establishes normal blood flow and avoids the need for emergency surgery. Another problem typically associated with balloon angioplasty is restenosis of a previously widened section of a blood vessel (in-stent restenosis). When balloon angioplasty results in a dissection forming inside a diseased vessel, this can lead to an overgrowth of scar tissue, which in turn can result in restenosis of a previously treated section. Although the introduction of stents has helped to counteract this problem, the use of bare metal stents is associated with restenosis in up to a third of all treated sections, with the exact rate of restenosis dependent upon the characteristics of the previously treated section (length of lesion, vessel diameter, degree of calcification). Brachytherapy and drug eluting stents were considered to be the potential treatment method for the treatment of ISR but were associated with risk of edge restenosis and late thrombosis. As the role of stents is temporary only till healing, reendothelialization and no benefits are found thereafter researchers have targeted the biodegradable and corrodible products used in medicine to develop biodegradable and bioabsorbable stents or Bioabsorbable vascular scaffolds [3-10]. Following Figure 1 shows the technological evolution with advantages and risks associated in Angioplasty treatment.
Bioresorbable Vascular Scaffolds (BVS)
Dramatic advances in Bioabsorbable materials and technology have delivered the potential for a fully absorbable scaffold, which is able to mechanically support the coronary artery for a predetermined time period. BVS represent a new concept of providing transient vessel support with drug delivery capability but theoretically without the long term limitations of metallic DES [11-15]. Such as permanent vessel caging and possible malapposition, risk of late ST, neoatherosclerosis, and local inflammation also permanent metallic stenting precludes the possibility of later surgical revascularization prevents late lumen enlargement, results in inhibiting non invasive imaging of coronary arteries using Computed tomography (CT) and Magnetic resonance imaging (MRI). Currently there are four materials used in BVS, of which lactide polymers particularly Poly-L-lactic acid form the basis of several devices and are the most extensively investigated other materials include magnesium poly anhydrates (salicylic acid and adipic acid) and poly carbonates (amino acids) [16-21]. Following Figure 2 shows how BVS implanted coronary blood vessel looks after complete degradation of stent material

Mechanism of Action of BVS
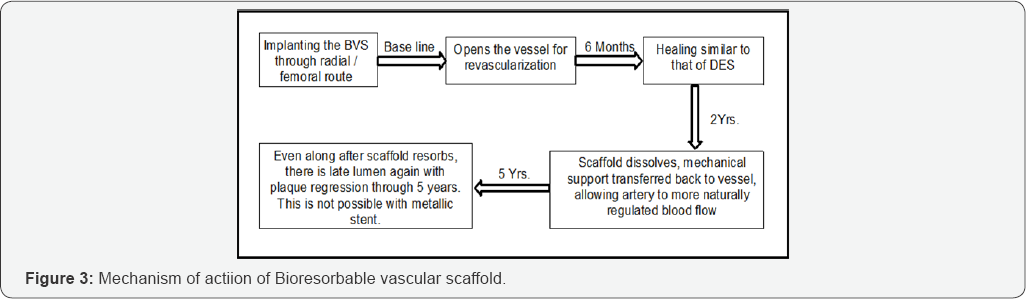
As a fully BVS, functions very differently than a metal stent- undergoing a series of physical changes, and leaving nothing behind. The revascularization phase is based on the principles of vascular restorative therapy (VRT)-that vessel radial support is needed for only a limited time. BVS provides the same vessel support and drug elution profile as the best-drug eluting stent [22-35]. Following Figure 3 shows the brief mechanism of action of BVS in an implanted coronary artery.
Advantages and Challenges of Bioresorbables Vascular Scaffolds
In the following Table 1, we represented the most important advantages and challenges associated with BVS.

Adverse Events Associated with BVS
From the clinical trials and real world experience of BVS, the adverse events that may be associated with treatment procedures and the use of a BVS in native coronary arteries include the following, but are not limited to allergic reaction or hypersensitivity to latex, device polymer and drug reactions to everolimus, anticoagulation or antiplatelet drugs, scaffold thrombosis (acute, subacute, late, very late), Stenosis or restenosis, including cardiac arrhythmias, cardiac ischemic conditions, cerebrovascular accident (CVA) and transient ischemic attack (TIA), system organ failures, cardiorespiratory arrest, and death [36-38].
Composition of BVS
The current BVS are composed of either a polymer or bioresorbable metal alloy. Numerous different polymers are available, each with different chemical compositions, mechanical properties and subsequently bioabsorption times. The most frequently used polymer in the current generation of BVS is PLLA. PLLA is already in widespread clinical use with applications such as resorbable sutures, soft-tissue implants, orthopedic implants, and dialysis media. The key mechanical traits for candidate material in coronary indications include high-elastic moduli to impart radial stiffness, large-break strains to impart the ability to withstand deformations from the crimped to expanded states and low-yield strains to reduce the amount of recoil and over inflation necessary to achieve a target deployment. Stent developers look to increase stent strut dimensions to compensate for mechanical shortcomings of bioresorbable materials. As the thickness of these struts increases, strain levels imposed on a material increase proportionally [39-42].
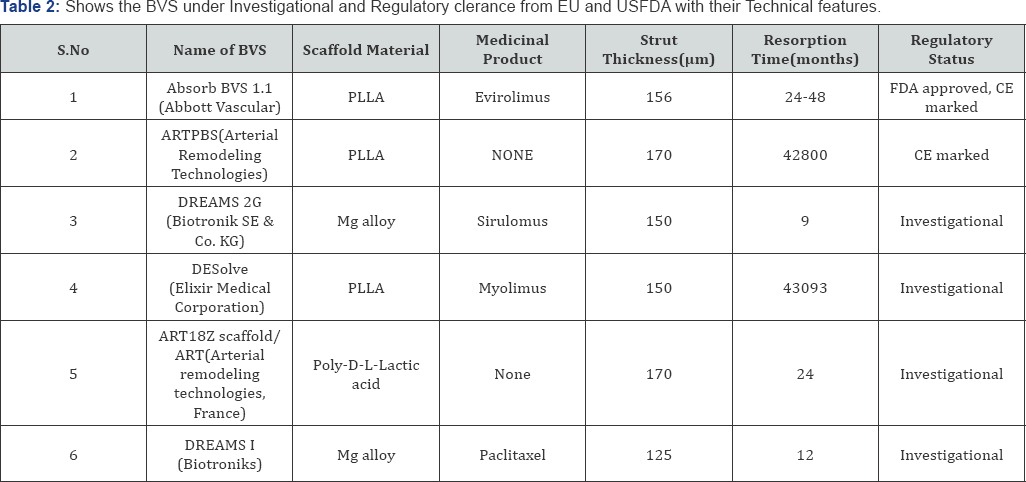
BVS under Investigational, CE Marked and USFDA Approved
The following Table 2 shows the BVS under Investigational and Regulatory clearance from EU and USFDA with their Technical features [43,44].
Issues Associated with the Marketed BVS
The Absorb everolimus-eluting bioresorbable vascular scaffold (Abbott Vascular) was approved for use by the Food and Drug Administration (FDA) in July 2016. The largest trial of the Absorb Bioresorbable scaffold was the ABSORB III trial, which included 2008 patients. In the ABSORB III trial, the bioresorbable scaffold was found to be non inferior to the Xience everolimus-eluting metallic stent (Abbott Vascular) with respect to the composite end point of target-lesion failure (cardiac death, target-vessel myocardial infarction or ischemia driven target-lesion revascularization) at 1 year (with a rate of 7.8% with the Absorb scaffold vs 6.1% with the Xience stent, P=0.007 for non inferiority). However, the rate of device thrombosis within 1 year after implantation was higher, although non significantly higher in the group that received bioresorbable scaffolds than in the group that received metallic stents (1.5% and 0.7%, respectively, P =0.13). In unpublished results at 2 years after implantation (reported at the 2017 meetings of the American College of Cardiology. The rate of target-lesion failure was significantly higher in the bioresorbable-scaffold group than the metallic-stent group (11.0% vs 7.9%, P =0.03 for superiority of the stent). These results show that BVS is generally comparable with the drug eluting stent when the device is placed in appropriately sized vessels and placed using appropriate procedural techniques. These findings have led the FDA to issue a safety alert for the Absorb bioresorbable vascular scaffold.
Current status of Marketed BVS
After the safety alerts from FDA Absorb BVS stents will no longer be supplying to non registry site in Europe that those sites should cease implantation and that remain BVS product will be removed by the Abbott vascular. With effective from May 31, 2017, the device will only be available in clinical register setting at selected sites or institutions that will play a pivotal role in the monitoring of this technology until summer 2018 at which time the situation will be reviewed [45]. Subsequently post marketing registries are being initiated in Europe and India to monitor implantation techniques for the Absorb dissolving stent, these E.U. registries will parallel post approval observational studies and training being conducted in other parts of the world including the ABSORB IV study of 3,000 Patients in the united states to conform the effect of current implantation technique on clinical outcomes [46-48].
Conclusion
With change in the life style of people affected by CAD and advanced in the technology for the treatment of CAD with interventional technologies for best outcomes, a hope is that a healed, normally functioning vessel free of foreign body and restenosis will be free of the risk of late thrombosis with the new generation devices like BVS.
Acknowledgment
Our special thanks to Prasanth .S, Blessy A. Daniel from S3V Vascular Technologies, Bangalore for their immense support and valuable suggestions throughout our review and we wish to thank our research guides, Prof. J. Vijaya Ratna, Dr. P. Shailaja, Andhra University College of Pharmaceutical Sciences for their effective guidance.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php
For more Open
Access Journals please click on: https://juniperpublishers.com
To know more about Juniper Publishers please click on: https://juniperpublishers.business.site/



Comments
Post a Comment