Pericarditis with Atrial Septal Defect with Bilateral Haemorrhagic Ovarian Cyst: A Case Report-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
We are reporting a case of bilateral haemorrhagic ovarian cyst with pericarditis with atrial septal defect (ASD) in a 32 years female. Diagnosis of ASD was incidental when she was under evaluation for bilateral haemorrhagic ovarian cyst. Diagnosis was confirmed by echocardiography. During closure of ASD, pericardium was not used for patch closure because pericardium was full of multiple small nodules which was a suspected case of tubercular pericarditis, patient had also bilateral ovarian cyst which was suspected due to TB. ASD was closed by using Polytetrafluroethylene (PTFE) patch. Pericardium was sent for histopathology and report was chronic pericarditis. Postoperative course was uneventful with marked improvement of symptoms
Introduction
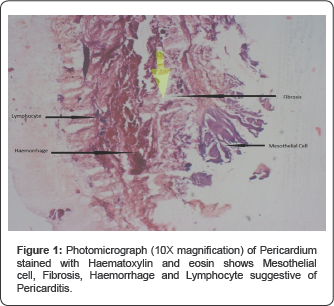
ASD is a common congenital heart disease. Secondum type of ASD occurs in 1 in 1500 live birth, accounting for 10% to 15%of congenital heart disease in children and 20 to 40% of defect discovered in adult [1]. Women are affected twice as often as men [1]. Association with other diseases or conditions can be found like migraine, stroke and diver's decompression illness [2-4]. Also there is association with other anomaly such as persistent left superior vena cava, mild or moderate pulmonary stenosis, azygos extension of Inferior vena cava, small Persistent ductus arteriosus, coarctation of aorta [5]. Here we present a case where patient was under treatment for ovarian cyst and ASD with Pericarditis was an incidental finding (Figure 1).
Case Present
A 32 year old presented with breathlessness since childhood. Dysmenorrhea and menorrhagia for 7 years. Patient also had lower abdominal pain for 1 year. The general examination revealed no anaemia, cyanosis, jaundice, clubbing, edema or dehydration. Cardiovascular examination showed normal 1st heart sound and fixed splitting of 2nd heart sound. There was a soft systolic flow murmur in pulmonary area. Patients Hb% 11.8 g/dl, ESR was 25mm in 1st hour, total W.B.C. count was 15000/cmm, Neutrophil 70%, Lymphocyte 25%, Monocyte 4%, Montoux test was negative, sputum for AFB was negative. Chest X ray showed mild cardiomegaly. A 2D and M mode echo showed large secondum type of ASD (25mm), and mild pulmonary hypertension (PASP 46mm of Hg) with dilated Right Atrium, Right Ventricle and Pulmonary Trunk. Cardiac catheterization done. There was step up of O2 saturation. Qp/Qs was 2:1.
Ultrasonography of the lower abdomen showed enlarged both ovaries containing multiple cysts- suggesting haemorrhagic cyst. Serum CA -19.9 was 17.3U/ml and CA -125 was 38.4u/ ml which was 3 units higher than normal reference range. The patient underwent surgical closure of ASD. The patient was placed in supine position. Anesthesia was given. Standard median sternotomy done. After pericardiotomy pericardium showed multiple whitish nodules in the inner surface of pericardium, also some thread like structure was found along with it. Cardiopulmonary bypass was established by bicaval cannulation. After attaining mild (32 °C) hypothermia cross clamp given on the aorta and ante grade cardioplegia was given. After right atriotomy ASD was found size about 30X20mm. ASD was closed using PTFE patch. Right atrium was closed in layers. Weaning from cardiopulmonary bypass was done without any difficulty. Pericardial biopsy was taken and sent for histopathology. Post-operative recovery was uneventful. Histopathology showed pericarditis.
Discussion
There are a few case reports on ASD with Pericarditis. Yoshihisa and colleagues found one case where transthoracic echocardiography demonstrated ASD but the finding of thickened pericardium was poor. Diagnosis was confirmed by catheterization. Pericardiotomy and direct closure of ASD was performed [6]. Harada and colleagues presented two cases of ASD with pericarditis where patients were 1 and 13 years old [7]. One patient died soon after surgery due to low cardiac output. The other patient was associated with protein-loosing enteropathy and it improved dramatically after operation [7]. Kanda & Naganuma [8] reported a case where signs of ASD were masked by those of pericarditis. Diagnosis was made by MRI and Doppler echo and confirmed by catheterization [8]. Tanaka& Murota [9] reported a case where ASD was missed at first operation because diagnosis of ASD was difficult [9]. We have experienced a surgical repair of ASD in 32 year female who also has bilateral ovarian cyst which was haemorrhagic type. Her ASD diagnosis was incidental. She was under gynecological consultation regarding ovarian cyst. Pre-operative echocardiography revealed ASD. Though she was having mild breathlessness on exertion she never took medical advice. Peroperatively pericardium was found full of multiple small nodules which was a suspected case of tubercular pericarditis, though histopathology showed pericarditis. Preoperative investigation could not diagnose pericarditis. Pericarditis is difficult to diagnose by investigations like echocardiography, cardiac catheterization.
Conclusion
Atrial septal defect is a congenital condition and is not related with pericarditis or bilateral haemorrhagic ovarian cyst. We present the case as it is a rare finding in our long experience.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php
For more Open
Access Journals please click on: https://juniperpublishers.com
To know more about Juniper Publishers please click on: https://juniperpublishers.business.site/



Comments
Post a Comment