Clinical Profile and Outcome of Infective Endocarditis in a Tertiary Care Centre: Retrospective Study-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Objective: This study was conducted
to outline the clinical profile and outcomes of infective endocarditic
(IE). It provides a contemporary picture of the presentation, etiology
and outcomes of IE.
Methods: A total of 97 consecutive
cases of definitive IE who met the modified Duke’s definitive criteria
were included in the study. We analysed their clinic-epidemiologic
features and outcomes.
Results: The mean age was 34.8±14.6
years with male preponderance (57.7%). Rheumatic heart disease (RHD)
(29.8%) was the commonest underlying cause followed by congenital heart
disease (CHD) (20.6%). Fever as the main clinical feature was seen in
95.8%. About 61.8% of patients were in New York Heart Association (NYHA)
class II. Blood culture was positive in 44.3% with commonest organisms
being Staphylococcus aureus (10.3%) and Streptococci viridians (9.3%).
Most common valve involvement was mitral valve (50.5%) followed by
aortic valve (38.14%). Eleven (11.33%) patients had right-sided cardiac
valve involvement. Complications were cardiovascular in 27 (27.8%) cases
congestive heart failure in 24.7%, atrioventricular block in (3.1%),
renal failure in 5 cases (5.2%) and neurological in 10 (10.30%) cases.
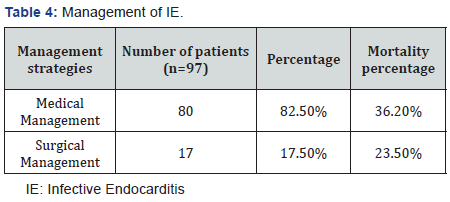
In-hospital mortality was high (34.1%). Only 17 (17.5%) patients
underwent surgery for IE.
Conclusion: Morbidity as well as
mortality is considerably high with IE. Staphylococcal infection is the
most common etiologic agent. RHD is the commonest underlying heart
disease in our population. Culture positivity rates and surgery for
infective endocarditis is low. Early cardiac surgery may help to improve
the outcomes in these patients.
Introduction
Infective endocarditis (IE) is a disease
characterized by high morbidity and mortality. Despite advances during
the past century in diagnosis [1,2], medical therapy [3] and surgical
treatment [4]. Mortality rates have not changed substantially in the
past 25 years. The current in-hospital mortality rate for patients with
IE is 15% to 20%, with1year mortality approaching 40% [5]. Majority of
patients in our clinical practice do not manifest all the classical
signs of endocarditis. Thus, a high index of clinical suspicion and
early investigation of those at risk is required. Echocardiography
remains central to the diagnosis of IE. The common differential
diagnosis in
our patients includes nodules due to acute rheumatic fever, ruptured
chordae, myxomatous degeneration, and thrombus. Other causes of
vegetation-like structures include neoplasia (atrial myxoma, marantic
endocarditis, papillary fibro elastoma, and carcinoid), auto immune
diseases (systemic lupus erythematosus, Wegener’s granulomatosis,
Behçet’s disease, and eosinophilic heart disease) and even normal
structures like Chiari malformation, and Lambl’s excrescences. The
sensitivity of transthoracic-echocardiography (TTE) is reported to be
40-63% [5]. The recent ACC guidelines [6] recommend the use of modified
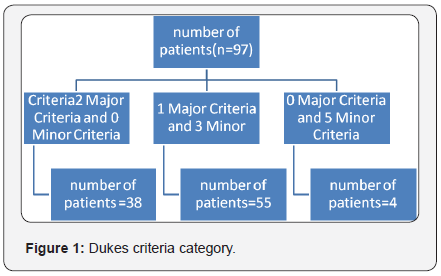
Dukes criteria as the primary scheme for the diagnosis of IE (Figure 1).
This study aims to outline the clinical profile and outcome
of infective endocarditis. It provides a contemporary picture
of the presentation, etiology, and outcome of infective
endocarditis (IE).
This is a retrospective observational study consisting of a
total of 97 consecutive cases of definitive infective endocarditis
(IE), admitted between January 2008 and May 2016, at Sri
Venkateswara Institute of Medical Sciences (SVIMS), Tirupati,
India. Patients who met the modified Duke’s definitive
criteria [7] for IE were included in this study. We analysed
patients clinic-epidemiologic features and outcomes. The data
regarding the clinical presentation, predisposing factors,
precipitating cause, investigative work up and outcome were
recorded.
All age groups of patients diagnosed as definitive infective
endocarditis based on modified Dukes criteria were included.
Patients who did not meet Dukes criteria, patients
unwilling to participate and no evidence of IE at surgery were
excluded from study.
Transthoracic Echocardiography (TTE): All patients
underwent TTE. Two dimensional and Doppler echo cardio
graphic studies were performed in the left lateral decubitus
position with conventional views (parasternal long, short axis
and apical 4 chamber view) according to the American Society
of Echocardiography guidelines [8]. Echocardiogram with
oscillating intra cardiac mass on valve, sub valvular structures,
site of impact of regurgitate jets, or on prosthetic material
without another alternatively anatomical explanation were
considered positive for IE. Other important echo cardio graphic
features which were considered positive for IE are abscess,
new prosthetic valve dehiscence or valvular regurgitation.
Blood Cultures
At least three blood culture samples (aerobic and anaerobic)
were obtained before initiation of antibiotic therapy. Blood
samples were drawn from different puncture sites (three
samples) separated apart by at least one hour if warranted
clinically, fungal cultures were also done.
Continuous variables are expressed as mean±SD.
Categorical variables are presented as frequencies and
percentages.
The mean age of IE patients was 34.8±14.6 years, with
highest concentration (23.7%) in the defined as age group of
31-40 years and with male preponderance (57.7%). Normal
systolic left ventricular function, defined as ejection fraction
(EF) ≥55% was seen in 59 cases (60.8%). Mild pulmonary
arterial hypertension (PAH) was present in 49 cases (50.51%).
Prior history of IE was found in 4 cases (4.1%) Most of the
cases (95%) had no prior antibiotic use before admission Fever
(95.9%) was the commonest presenting symptom and physical
sign pallor (32.9%) was the second common physical finding.
New York Heart Association (NYHA) Class-II was found in
61.85% of the study subjects Hypertension (8.2%) was the
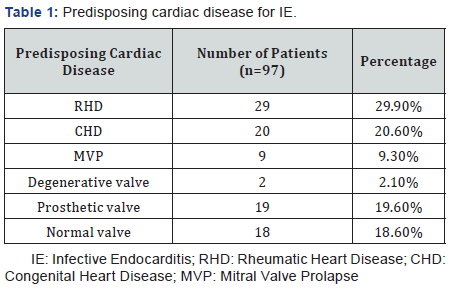
most common associated clinical condition. Rheumatic heart
disease (RHD) (29.9%) was the commonest underlying cause
followed by congenital heart disease (CHD) (20.6%) (Table
1). Bicuspid aortic value (55%) was the most common CHD
causing IE. Most common valve involvement was found to be
mitral valve (50.5%) followed by aortic valve (38.1%). Eleven
(11.3%) patients had right-sided cardiac valve involvement.
Vegetations were present in 93 cases (95.9%). Mitral
regurgitation (42.3%) was the most common abnormality
found on echocardiography. Single vegetation was found
in 83 cases (89.3%) and size of ≤5mm was seen in 61 cases
(66.7%). Perivalvular abscess was seen in 3 cases of whom two
had prosthetic valve and one had congenital bicuspid valve.
Blood culture was positive in 44.3% of cases with commonest
cultured organisms being Staphylococcus aureus (10.3%) and Streptococci viridians (9.3%). Negative blood culture was
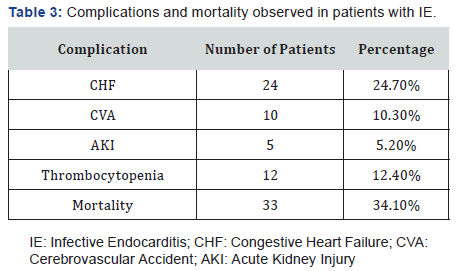
found in 54 cases (57.7%) (Table 2). Complications associated
with IE were cardiovascular in 27 (27.8%) cases (congestive
heart failure in 24.7%, atrioventricular (AV) block in 3.1%),
renal failure 5 cases (5.1%), neurological in 10 cases (10.3%)
and in-hospital mortality remained high (34.02%) (Table 3).
Congestive heart failure was seen in 24 cases. Of these mitral
valve was involved in 6 cases, aortic valve was involved in 3
cases and both mitral and aortic valve were involved in 15
cases. Cerebral embolism was found in 10 cases (10.3%), mean
size of the vegetation seen in these cases was 12±3mm and
were highly mobile with involvement of mitral valve in 6 cases
and aortic valve in 4 cases. Peripheral embolism was seen in
5 cases (5.15%). AV block was seen in 3 cases of which mitral
valve was involved in one case and aortic valve in two cases.
Only 17 (17.5%) patients underwent surgery for IE (Table 4).
A total of 80 patients were managed medically out of which 29
died. Most of these cases (n=18) presented in NYHA IV with
cardiogenic shock. Mortality with medical management was
29 cases (36.2%) while with surgical management was 4 cases
(23.5%).

The current scenario of IE has changed owing to multitude
of possible factors which include empirical or indiscriminate
use of antibiotics therapy, increasing population of elderly age
group, prosthetic devices/pacemaker leads implantation and
increasing healthcare acquired infections. The mean age of
our patients was 34.8 years and 63.9% of our patients were
younger than 40 years which is very similar to the previous
Indian studies [9-11]. The lower mean age is attributable to the
fact that, this study also included the paediatric population.
Also, RHD which continues to be a rampant problem in the
underprivileged population in India predominantly affects
younger age group [12].
RHD was the most common underlying heart disease in
present study which accounted for 29.9% of all cases, which
is similar to other Indian studies [9]. In rheumatic valavulitis
focal nodular thickening of the body and tips of the leaflet is
important feature that can be picked up by echocardiogram.
These nodules are 3-5mm in size and have different echogenicity
from the valve structures and do not have the characteristic
mobility of endocarditic vegetations. These are considered
rheumatic verucae equivalents and are seen commonly in the
mitral valve; these can be seen on tricuspid and aortic valve
also rarely. These verucae need to be differentiated from
vegetations of endocarditis.
CHD accounted for 20.6%. This high incidence of CHD
in our study is in contrast to a large multi-centric study by
Murdoch et al. [12] in which CHD constituted 12% of IE cases
[13]. Bicuspid aortic valve is the most common congenital
etiology for infective endocarditis in infants and children. The
risk of developing infective endocarditis on a bicuspid aortic
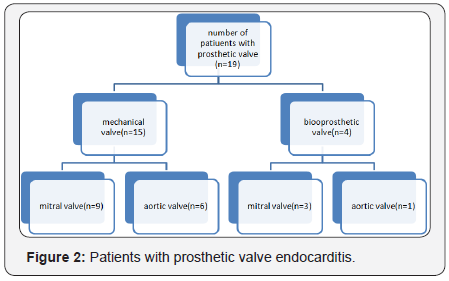
valve is 10-30% over lifetime [14]. In our study, prosthetic
valve endocarditis (PVE) constituted 19 (19.6%) cases of IE
which is very similar to other western studies but higher than
some previous Indian studies [9,15,16] (Figure 2). Incidence
of PVE has increased in India from 1% in 1980’s to 10% in
1990’s [10]. Diagnosis of prosthetic valve endocarditis by the
TTE is more difficult because multitude of various imaging
artefacts (reverberations, attenuation etc.) can occur with
both mechanical and bio prosthetic valves. Particularly in
the case of a mechanical valve, TTE may be helpful only when
there is large or mobile vegetation or significant regurgitation.
These limitations are resolved with the use of transesophageal imaging techniques because of the superior imaging quality
and posterior transducer position. In contrast to the western
data in which mitral valve prolapsed (MVP) was reported to
be a common underlying heart lesion, this group constituted
9 (9.3%) patients in our study. Although it is traditionally
believed that IE does not affect normal valves, recent large
series have reported no underlying structural heart disease
in about a third of patients [17]. In our study 18(18.6%) of
patients had no structural heart disease.
Echocardiography has proved the most important tool in
establishing diagnosis of IE in our study. This is especially due
to the low culture positivity rates. Vegetations were detected
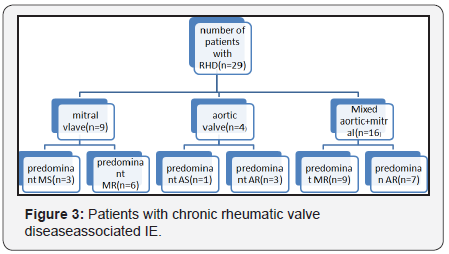
by TTE in 93 (95.9%). The most common site of vegetations
in our study was mitral valve followed by aortic valve which
is similar to study by Garg et al. [10] and other Indian studies
[9] (Figure 3). A low culture positivity rate noted in our study.
Optimal therapy of IE depends on the organism isolated on
culture and their sensitivity patterns. This is similar to the
study done by Sharad et al. [18]. Ninty three patients had no
previous history of antibiotic use. Blood cultures were positive
only in 44 cases, this may be because of under reporting of
previous antibiotic use [19]. Recent data from the west series
has shown there has been a shift in the microbiological spectrum
with Staphylococcusbeing the commonest isolate [20]. In our
study also the most common isolate was Staphylococcus aurous
followed by Streptococci viridians. Staphylococcus aureus is now
the most common cause of IE in much of the world, according to
several recent investigatiors [21]. However, the previous Indian
study by Garg et al. [10] had shown Streptococci as the most
common isolate. The increasing emergence of Staphylococcus
is due to an increasing geriatric population, rising drug abuse,
increasing nosocomial infections and use of prosthetic devices.
A negative blood culture not only delays the diagnosis, but also
misclassifies the patient precluding appropriate antibiotics.
IE due to atypical organisms should be considered in negative
blood culture cases in immuno compromised, renal failure and
patients with impanted prosthetic devices/pacemaker leads
and intravenous dwelling catheters [20].
In our study, the in-hospital mortality was 33 (34.1%)
which is much higher than that reported in the recent studies
(12.6%-17.7%) [13,22]. This may have occurred probably due
to the complicated and refractory group of patients referred
to our centre. Further contributing was delayed presentation
of patients to the hospital. Also high culture negative rates and
lower rates of surgery 17 (17.5%) may be contributory.
This is single centre retrospective study. Small sample
size. Only in hospital outcomes were taken in the study and
long-term follow-up is absent.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment