A Study of 1,236 Patients Supporting the Use of Unfractionated Heparin With or Without Glycoprotein IIb/IIIa Inhibitors over Bivalirudin in Primary Percutaneous Coronary Intervention for ST-Segment Elevation Myocardial Infarction: A Changing Trend-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Background
The use of antithrombotic therapy such as heparin and
bivalirudin are standard of practice in managing ST-segment elevation
myocardial infarction patients undergoing primary percutaneous coronary
intervention with a Class I recommendation. Recently the American
College of Cardiology published in JACC: Cardiovascular Interventions a
study analyzing the trends in anticoagulant use among 513,775 PCIs for
STEMI from July 2009 through December 2014 utilizing information
available from the National Cardiovascular Data Registry CathPCI
Registry. In this study, bivalirudin was associated with a reduction in
adverse bleeding events attributed to an increased use of glycoprotein
IIb/IIIa inhibitors (GPI) alongside UFH.
Objective: To report the efficacy and safety outcomes of UFH with routine use of GPI in primary PCI for STEMI in a high-risk population.
Methods: Single center,
retrospective chart review of 1,236 adults undergoing primary PCI.
Patients were followed up for 30 days. The primary efficacy outcome was a
composite of all-cause mortality, cerebrovascular accident,
reinfarction, or stent thrombosis. The primary safety outcome was a
composite of access site and non-access site incidence of bleeding.
Results: The rate of MACE was
3(0.2%) with stent thrombosis, any bleeding event in 30(2.5%), new
myocardial infarction or reinfarction in 7(0.5%) and mortality rate
(4%).
Conclusion: In our study UFH with
GPI demonstrated a decrease in the rates of stent thrombosis, adverse
bleeding events, and new myocardial infarction or reinfarction when
compared to RCTs and international registries.
Abbreviations: CPX: Cardio-Pulmonary Exercise stress test; VC: Vital Capacity; MVV: Maximum Voluntary Ventilation; SaO2: Arterial Oxygen Saturation; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; MHR: Maximum Heart Rate; BMI: Body Mass Index; HDL-C: High-Density Lipoprotein- Cholesterol; TC: Total Cholesterol
Introduction
For patients with STEMI undergoing primary PCI the
following anticoagulation regimens are recommended as Class I:
Unfractionated Heparin (UFH) with additional boluses administered to
maintain therapeutic activated clotting times (ACT) or bivalirudin with
or without previous treatment with UFH. The guidelines also state with
Class II level of
recommendation that in patients with STEMI undergoing PCI who are at
high risk of bleeding, it is reasonable to use bivalirudin monotherapy
in preference to the combination of UFH and a GPI.
Bivalirudin use increased substantially in the United
States from 2010 till 2014 compared to UFH monotherapy and UFH plus GPI
[1]. However, the use of bivalirudin is not a universal practicedue to
the concerns of increased risk of stent thrombosis [2,3].
In 2014, HEAT PPCI study showed UFH to be equally efficacious
and safer as compared to bivalirudin [4]. Since HEAT PPCI was
published in 2014 bivalirudin usage decreased substantially
and UFH monotherapy as well as UFH plus GPI usage increased
changing the trend back in favor of UFH in STEMI [1]. More
importantly based in our individual center experience the actual
bleeding rates with UFH plus GPI are lower than those reported
in randomized controlled trials (RCTs) and in line with recent
study published in JACC: Cardiovascular Interventions [1]. Our
center predominantly uses UFH plus GPI. In this study we aimed
to review our single center experience with the cautious use
of GPI’s in addition to UFH in a high-risk population including
patients with high risk angiographic features, advanced heart
failure, previous MIs and significant comorbid conditions with a
real world experience.
In recent years the use of radial artery access has increased
dramatically in STEMI patients undergoing intervention,
favorable affecting adverse bleeding events. The use of vascular
closure devices has helped achieve rapid closure of the femoral
access site. Monitoring ACT and choosing low dose Heparin
boluses has improved bleeding outcomes. All these points raise
an important question of real indications for bivalirudin; a
drug associated with an increased rate of stent thrombosis and
limited mortally benefit.
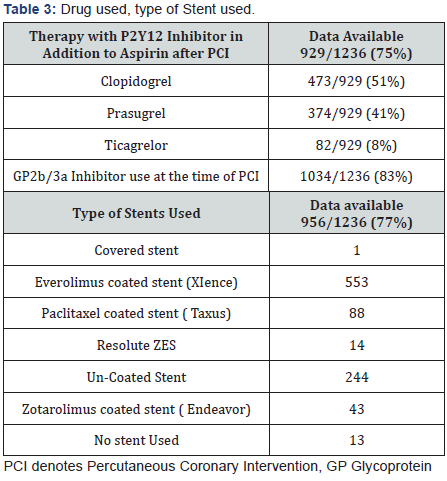
Between June 2009 and April 2015 a total of 1,236 patients
underwent primary PCI for STEMI in our tertiary care center.
Aspirin naive patients were loaded with 324mg aspirin preprocedure
along with a 3000-4000 IU IV bolus of Heparin. During
the procedure we continued with IV Heparin boluses while
monitoring ACT and 83% of patients also received GPI. Patients
were prescribed clopidogrel (loading dose, 300 or 600mg) or
Prasugrel 60mg or Ticagrelor 90mg after the PCI. Dual antiplatelet
therapy was given daily to all patients during their index hospital
stay and was then continued indefinitely. Outcomes observed
were stent thrombosis, bleeding rates, reinfarction, stroke, and
thirty-day mortality. Baseline characteristics of the study group
are listed in Table 1. Mean age of our patient population was
66 years and 975(78%) were males. Comorbidities included
772(62%) with hypertension, 422(34%) diabetes, 546(44%)
hyperlipidemia, and 529(42%) had a smoking history. Available
data from 1,182 patients showed that left ventricular ejection
fraction was >55% in 192(17%), 45-54% in 302(25%), 35-44%
in 392(33%), and less than 35% in 296(25%) of patients. The
rate of MACE was limited to 3(0.2%) with stent thrombosis,
any bleeding event in 30(2.5%), new myocardial infarction or
reinfarction in 7(0.5%) and a total mortality rate of (4%). In the
landmark HEAT-PPCI trial, they recruited a near “all-comers”
population. The observed adverse event rates more closely
matched institutional norms and the results reported by national
registries. Their death rate was 4.3%, cerebrovascular accident
post PCI of 1.2%, new myocardial infarction or reinfarction of0.9%, stent thrombosis 0.9%, and any bleeding event rate of
13.5% in the Heparin arm of the trial.

The longstanding debate between heparin or bivalirudin in
primary percutaneous coronary intervention usually balances
the increased risk of stent thrombosis found with bivalirudin
versus the increased risk of bleeding with UFH plus GPI. We
believe that ACT guided dosing of Heparin, decreased duration
of therapy with a glycoprotein IIb/IIIa inhibitor, radial artery
access site, and frequent use of a closure devices in femoral
access dramatically decrease the bleeding rates while using UFH
in patients undergoing PCI.
Also data from the European Society of Cardiology showed
that adding a GPI to UFH might be beneficial in patients
presenting early with a large myocardial infarction and high
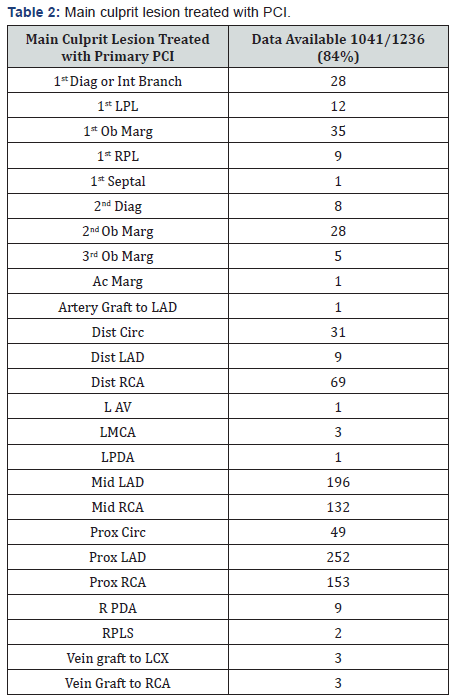
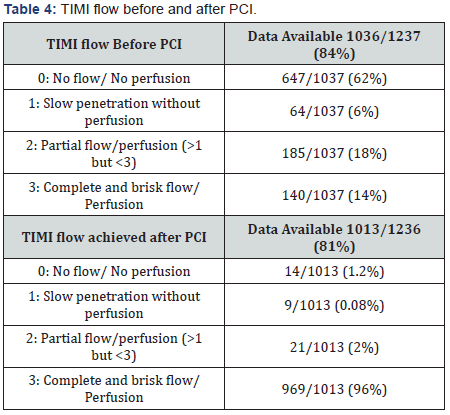
thrombus burden [5]. Main culprit lesion treated with PCI, drugs
used, type of stent used and Timi flow can be found on Table 2,
3 & 4.
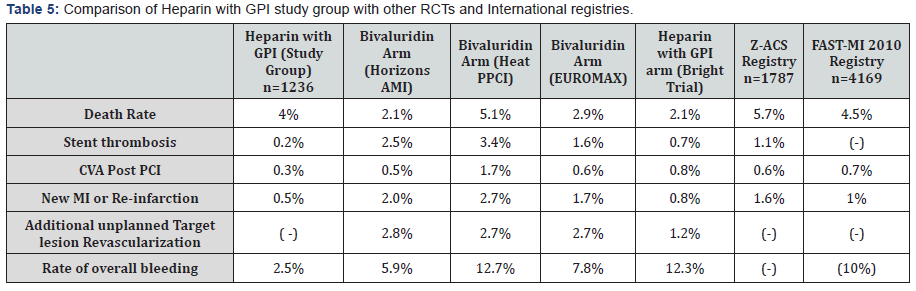
Our results predominantly using UFH and GPI in STEMI
patients undergoing primary PCI shows decreased stent
thrombosis, bleeding, and new myocardial infarction or
reinfarction rates as compared to both RCTs and international
registries (Table 5). Our PRBC transfusion rates of 2% were
comparable to landmark RCTs and international registries. Our
death rate of 4% was lower than in real world registries but
higher than RCTs.
Methods
Data was obtained through electronic medical records and
notes from health care providers. We utilized proportions,
percentages, frequency counts, measures of central tendency,
measures of variability, as well as various graphs and tables
to report on our descriptive research observations. Since data
abstractors who review and code each chart play an important
role with respect to data quality, we promoted that coding be
performed accurately and consistently, not to compromise the
validity of the data to be analyzed. Data abstractors remained
blinded to the purpose of the study.
Stent thrombosis and bleeding rates are associated with an
increased mortality and clinical practice is based on a balance of
this risk. UFH plus GPI use has increased bleeding rates in most
trials however we found the therapy to be efficacious as seen in
RCTs but more importantly we observe it to be associated with
fewer bleeding complications than previously reported. This
difference could stem from the lower doses of Heparin used,
length and choice of GPI therapy, careful ACT monitoring, and
frequent use of closure devices. The benefit of bivalirudin seen in
trials is driven by a decreased bleeding rate at the expense of an
increased incidence of stent thrombosis [6]. This benefit is likely
to decrease with time as intervention techniques and technology
advances occur such as the use of vascular closure devices and
transradial access. Studies have also shown bivalirudin having
no difference in adverse bleeding rates when compared to
UFH plus GPI utilizing transradial access [1]. RCTs have shown
bivalirudin to have a fivefold increased risk of stent thrombosis
[2,3]. In the Horizon AMI trial, approximately 65% of patients
received Heparin and analysis showed that randomization to
Heparin and a 600mg clopidogrel loading dose were independent
predictors of reduced acute and sub-acute stent thrombosis.
The increased risk of stent thrombosis in the bivalirudin arm
could be explained by its shorter half-life, however, the matrix
Trial comparing bivalirudin with unfractionated Heparin in
acute coronary syndrome failed to show any added advantage
of an extended infusion of bivalirudin. More importantly the
mace rates were not lower with bivalirudin, thus nullifying any
advantage over heparin [7,3]. In the Euromax trial there was no
mortality benefit at 30 days unlike Horizon trial, which showed
the benefit but was not powered appropriately [2-4].
Our study shows a significantly lower incidence of stent
thrombosis of 0.2% and overall bleeding rate of 2.5%. These
results are very encouraging when compared to bleeding and
stent thrombosis rates during the Heat PPCI and Bright trials [8-
12]. We believe that a shorter length of GPI therapy restricted
to equal or less than 16 hours with either Abciximab, Tirofiban
or Eptifibatide, cautious heparin dosing with ACT monitoring
ranging between 250-320 seconds, post-procedure 4-6 hour
bed rest and frequent use of a closure devices significantly
impacts adverse bleeding events. All these points question theutility of bivalirudin; a drug associated with an increased rate
of stent thrombosis and limited mortally benefit. Hence the
trend of use for bivalirudin has decreased recently with most
centers switching back to UFH with or without a GPI [1,13-
15]. We cannot ignore the lesser bleeding rates reported with
bivalirudin in Horizon AMI, EUROMAX, MATRIX, and other
trials [2,3,7]. Perhaps the limited advantage of bivalirudin could
be useful in select patients with a higher risk of bleeding. In
patients presenting early with high-risk angiographic features
and high thrombus burden, UFH plus a GPI was shown to be
a safe and effective therapy during primary PCI for high-risk
STEMI patients. Seeing our encouraging results we solely cannot
switch or recommend routine use of bivalirudin when compared
to unfractionated Heparin.
The death rate was reported to be 4%. Compared to the
landmark RCTs this number is slightly higher, but we would
like to stress that our population was older, had significantly
more patients with advanced heart failure, previous MIs, and
significant comorbid conditions with a real world experience.
Also most of our patients were treated with a GPI that would
generally increase bleeding. In spite of these measures our
bleeding rates were below expected range as compared to RCTs
and international registries.
A limitation of our study is that it is a retrospective chart
review and we have used randomized trials and registries as
cohort controls. We don’t have information on the incidence
of thrombocytopenia and bleeding rates at 30 days. However
stent thrombosis and bleeding complications are commonly
seen within the first 72 hours post procedure and reported in
our study. We don’t have data on post procedure bed rest, %
of closure device usage versus manual compression to achieve
hemostasis, or duration of GPI post procedure. Nevertheless it
is routine practice in our institution to have post procedure bed
rest for 4-6 hours, and GPI infusion limited to equal or less than
16 hours. The use of closure devices for femoral access is routine
in our institution as long as the arterial puncture site is below
the inguinal ligament and above the femoral bifurcation.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment