Salt, Glucose, and Hypertension: Interactions, Benefits and Risk-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Both dietary salt and sugar are related to blood
pressure (BP) and hypertension. The evidence for salt was initially
considered stronger, and various types of studies have consistently
shown that salt is a major cause of raised BP, and a reduction from the
current intake of between 9-12g/day in most countries of the world to a
recommended level of no more than 6 gram (i.e. 2.5 grams of sodium) on a
daily basis (an approximate of 1 teaspoon of salt per day) will lower
BP in both hypertensive and normotensive individuals, in men and women
of all age groups and in all the black and the Caucasians. The
physiology by which salt raises causes hypertension has to do with the
kidney using a delicate balance of sodium and potassium to pull water
across a wall of cells from the bloodstream into a collecting channel
that leads to the bladder. A high salt intake raises the amount of
sodium in the bloodstream and distorts this delicate balance, thereby
reducing the ability of the kidneys to remove the water. This causes
fluid retention which increases the pressure exerted by the blood
against blood vessel walls (high blood pressure). The sugar also is a
factor that increases BP. It is in fact, recently considered that sugar
may have more devastating effect of BP than salt. The mechanism by which
sugar interacts with BP has to do with insulin and leptin levels in the
body. It causes blood pressure to increase, and eventually, there may
become insulin and/or leptin resistant. Insulin stores magnesium, but if
its receptors are blunted and the cells grow resistant to insulin, the
body can’t store magnesium, so it passes out of the body through
urination. Magnesium stored in the cells relaxes muscles. If its level
is too low, the smooth muscle of the blood vessels will be unable to
fully relax, and this constriction raises blood pressure. The current
high intake of added sugars increases obesity which, in turn, raises BP.
Recent studies also suggest that added sugars, particularly those in
soft drinks, may have a direct effect on BP. Actions to reduce salt and
sugar intake across the world population have been recommended in this
review, and will go a long way to having beneficial effects on health
along with major cost savings from treatments.
Introduction
Blood pressure
Blood pressure is the force of blood against the
walls of arteries. Blood pressure has two components: the systolic
pressure (which is the force that blood exerts on the artery walls when
the heart pumps), and the diastolic pressure (which is the residual
force that remains when the heart relaxes between beats).
The measurement is written one above the other, with
the systolic number on top and the diastolic number on the bottom. For
example, a blood pressure measurement of 130/85mmHg (millimeters of
mercury) is expressed verbally as «130 over 85». The systolic is 130 and
the diastolic is 85.
Blood pressure varies from person to person and by age. In general: Normal blood pressure is less than 130mmHg systolic
and less than 85mmHg diastolic. Optimal blood pressure is less than 120mmHg systolic and less than 80mmHg diastolic.

*For those not taking medicine for high blood pressure and not
having a short-term serious illness. These categories are from the
National High Blood Pressure Education Program.
**Optimal blood pressure with respect to heart disease risk is below
120/80mm Hg. However, unusually low readings should be evaluated
for clinical significance.
<: Less than
≥: Greater than or equal to
Hypertension is generally defined as a blood pressure
greater than 140/90mmHg. Blood pressure should be brought
closer to what’s considered optimal: 120/80. An elevated blood
pressure raises the risk for heart attack and stroke. Depending
on other risk factors, even the high end of normal may be too
high for some people (Table 1).
There are two primary hypertension types. For 95
percent of people with high blood pressure, the cause of their
hypertension is unknown; this is called Essential or Primary
hypertension. When a cause can be found, the condition is
called Secondary hypertension.
Essential hypertension: This type of hypertension is
diagnosed after blood pressure remains high after about three
or more measurements and all other causes of hypertension are
eliminated. Usually people with essential hypertension have no
symptoms, but may experience frequent headaches, tiredness,
dizziness, or nose bleeds. Although the cause is unknown,
researchers have observed that obesity, smoking, alcohol, diet,
and heredity all play a role in essential hypertension.
Secondary hypertension: The most common cause of
secondary hypertension is an abnormality in the arteries
supplying blood to the kidneys. Other causes include airway
obstruction during sleep, diseases and tumors of the adrenal
glands, hormone abnormalities, thyroid disease, and too
much salt or alcohol in the diet. Drugs can cause secondary
hypertension, including over-the-counter medications such
as ibuprofen (Motrin, Advil, and others) and pseudoephedrine
(Afrin, Sudafed, and others). If the cause is found, hypertension
can often be controlled.
Additional hypertension types: isolated systolic,
malignant, and resistant
Isolated systolic hypertension, malignant hypertension,
and resistant hypertension are all recognized hypertension
types with specific diagnostic criteria.
Isolated systolic hypertension: Blood pressure is
recorded in two numbers: The upper, or first, number is
the systolic pressure, which is the pressure exerted during
the heartbeat; the lower, or second, number is the diastolic
pressure, which is the pressure as the heart is resting between
beats. Normal blood pressure is considered under 120/80.
With isolated systolic hypertension, the systolic pressurerises above 140, while the lower number stays near the normal
range, below 90. This type of hypertension is most common in
people over the age of 65 and is caused by the loss of elasticity
in the arteries. The systolic pressure is much more important
than the diastolic pressure when it comes to the risk of
cardiovascular disease for an older person.
Malignant hypertension: This hypertension type occurs
in only about 1 percent of people with hypertension. It is more
common in younger adults, African-American men, and women
who have pregnancy toxemia. Malignant hypertension occurs
when the blood pressure rises extremely quickly, with the
diastolic pressure going over 130. Symptoms include numbness
in the arms and legs, blurred vision, confusion, chest pain, and
headache.
Resistant hypertension: This is when a high blood
pressure remains high even after three different types of
antihypertensive medications are administered to a patient.
Resistant hypertension may occur in 20 to 30 percent of high
blood pressure cases. It may have a genetic component and is
more common in people that are older, obese, female, African-
American, or have an underlying illness, such as diabetes or
kidney disease.
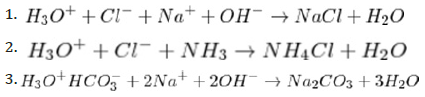
Salts: Salts are compounds made up of cations (e.g., K+, Ca2+,
NH4+) and anions, such as chloride (Cl-), nitrate (NO3-, that are
held together by ionic bonds. They are crystalline materials.
Salts normally consist of positively charged ions, cations,
and negatively charged ions, anions, that form a crystal lattice.
In addition, some salts may include the water molecule (H2O)
in the lattice; they are referred to as hydrated salts (Figure 1).

Salts, by definition, are the result of a neutralization
reaction, i.e., the mixture of an acid with a base.
Base + Acid → Salt + Water
While some salts, such as NaCl are neutral, that is, their
solution does not change the normal pH 7 of water, other saltsmay be alkaline or acidic, depending on the strength of the
participating acids and bases:
Salts may have different solubilities; while some salts are
very soluble, others may be practically insoluble. In general,
soluble salts are more «damaging» to inorganic porous
materials than the less soluble ones.
The formula for sodium chloride, NaCl, indicates that equal
numbers of sodium and chlorine atoms combine to form the
salt. Ionically, in the reaction of sodium with chlorine, each
sodium atom loses an electron, becoming positively charged,
and each chlorine atom gains an electron, becoming negatively
charged; there are equal numbers of positively charged sodium
ions and negatively charged chloride ions in sodium chloride.
The ions in a solid salt are usually arranged in a definite
crystalline structure, each positive ion being associated with a
fixed number of negative ions, and vice versa.
A salt that has neither hydrogen (H) nor hydroxyl (OH) in
its formula, e.g., sodium chloride (NaCl), is called a normal salt.
A salt that has hydrogen in its formula, e.g., sodium bicarbonate
(NaHCO3), is called an acid salt. A salt that has hydroxyl in its
formula, e.g., basic lead nitrate (Pb[OH]NO3), is called a basic
salt. Since a salt may react with a solvent to yield different ions
than were present in the salt, a solution of a normal salt may be
acidic or basic; e.g., trisodium phosphate, Na3PO. In addition to being classified as normal, acid, or basic, salts
are categorized as simple salts, double salts, or complex salts.
Simple salts, e.g., sodium chloride, contain only one kind of
positive ion (other than the hydrogen ion in acid salts). Double
salts contain two different positive ions, e.g., the mineral
dolomite, or calcium magnesium carbonate, CaMg(CO3)2. Alums
are a special kind of double salt. Complex salts, e.g., potassium
ferricyanide, K3Fe(CN)6, contain a complex ion that does not
dissociate in solution. A hydrate is a salt that includes water
in its solid crystalline form; Glauber’s salt and Epsom salts are
examples of hydrates.
Salts are often grouped according to the negative ion they
contain, e.g., bicarbonate or carbonate, chlorate, chloride,
cyanide, fulminate, nitrate, phosphate, silicate, sulfate, or
sulfide.
Sugar is the generalized name for sweet, short-chain,
soluble carbohydrates, many of which are used in food. They
are composed of carbon, hydrogen, and oxygen. There are
various types of sugar derived from different sources. Simple
sugars are called monosaccharides and include glucose (also
known as dextrose), fructose, and galactose. The table or
granulated sugar most customarily used as food is sucrose,
a disaccharide. In the body, sucrose hydrolyses into fructose
and glucose. Other disaccharides include maltose and
lactose. Longer chains of sugars are called oligosaccharides.
Chemically, different substances may also have a sweet taste,
but are not classified as sugars. Some are used as lower-calorie
food substitutes for sugar described as artificial sweeteners.
Studies in animals have suggested that chronic
consumption of refined sugars can contribute to metabolic
and cardiovascular dysfunction. Some experts have suggested
that refined fructose is more damaging than refined glucose
in terms of cardiovascular risk. Cardiac performance has been
shown to be impaired by switching from a carbohydrate diet
including fiber to a high-carbohydrate diet [1]. Switching from
saturated fatty acids to carbohydrates with high glycemic
index values shows a statistically-significant increase in the
risk of myocardial infarction [2]. Other studies have shown
that the risk of developing coronary heart disease is decreased
by adopting a diet high in polyunsaturated fatty acids but low
in sugar, whereas a low-fat, high-carbohydrate diet brings
no reduction. This suggests that consuming a diet with a
high glycemic load typical of the «junk food» diet is strongly
associated with an increased risk of developing coronary heart
disease [3].
The consumption of added sugars has been positively
associated with multiple measures known to increase
cardiovascular disease risk amongst adolescents as well as
adults [4]. Studies are suggesting that the impact of refined
carbohydrates or high glycemic load carbohydrates is more
significant than the impact of saturated fatty acids on
cardiovascular disease [5,6]. A high dietary intake of sugar (in
this case, sucrose or disaccharide) can substantially increase
the risk of heart and vascular diseases.
Interactions: It has been established in chapter one
that blood pressure is the relationship between the amount
of blood ejected from the heart with each heartbeat and the
resistance against which it ejects, and that systolic blood
pressure is the peak pressure generated by the volume of blood
ejected and diastolic pressure the pressure in blood vessels
during the period between heartbeats (the time the heart fills
with blood between beats is called «diastole»). The cardiac
output is determined by the amount of blood in the heart atthe beginning of a beat and so is dependent on the total blood
volume.
Arthur Guyton, a physiologist had postulated the theory
of «pressure natriuresis». It basically states that every patient
with high blood pressure has a disorder of salt handling by the
kidney. The appropriate response to increased blood pressure
is increased salt excretion through the kidney. A large body of
experimental data does indeed point to abnormally slow salt
excretion by the kidney as an important component of human
hypertension [7].
Cogent evidences indicate that salt intake is strongly related
to the development of hypertension, particularly the rise in
blood pressure with age [7]. The risk of cardiovascular disease
increases throughout the range of blood pressure starting
from a systolic blood pressure of 115mmHg [8,9] which 80%
of the adult population exceeds. Raised blood pressure is the
major cause of the development of cardiovascular disease, and
accounts for 60% of all strokes and 50% of all heart disease
[10]. Blood pressure is the biggest cause of death in the world
through the strokes and heart attacks it causes.
How salts specifically interact with blood pressure
(Hypertension): The kidney uses a delicate balance of sodium
and potassium to pull water across a wall of cells from the
bloodstream into a collecting channel that leads to the bladder.
A high salt intake raises the amount of sodium in the
bloodstream and wrecks the delicate balance, reducing the
ability of the kidneys to remove the water. This causes fluid
retention which increases the pressure exerted by the blood
against blood vessel walls (high blood pressure).
On the arteries: The extra blood pressure caused by eating
too much salt puts extra strain on the insides of the arteries. To
cope with the extra strain, the tiny muscles in the artery walls
become stronger and thicker. Yet this only makes the space
inside the arteries smaller and raises the blood pressure even
higher.
This cycle of increasing blood pressure (which occurs
slowly over a number of years) can ultimately lead to the
arteries bursting or becoming so narrow that they then clog up
entirely. When this happens, the organs of the body that were
receiving the blood from the arteries become starved of the
oxygen and nutrients they need. This can result in the organs
being damaged.
On the heart: The raised blood pressure caused by eating
too much salt may damage the arteries leading to the heart.
At first, it may cause a slight reduction in the amount of blood
reaching the heart. This may lead to angina (sharp pains in the
chest when being active).
With this condition, the cells in the heart don’t work as well
as they should because they are not receiving enough oxygenand nutrients. However, lowering blood pressure may help to
alleviate some of the problems and reduce the risk of greater
damage.
But if the salt intake is not controlled over time, the
damage caused by the extra blood pressure may become so
severe that the arteries burst or become completely clogged.
If this happens, then the part of the heart that was receiving
the blood no longer gets the oxygen and nutrients it needs and
dies. The result is a heart attack. The best way to prevent a
heart attack is to stop the arteries becoming damaged. And one
of the best ways of doing this is keep the blood pressure down
by eating less salt.
On the brain: The raised blood pressure caused by
increased intake of salt may damage the arteries leading to the
brain. At first, it may cause a slight reduction in the amount of
blood reaching the brain. This may lead to vascular dementia.
With this condition, the cells in the brain don’t work as
well as they should because they do not receive enough oxygen
and nutrients. However, lowering blood pressure may help to
alleviate some of the problems and reduce the risk of greater
damage.
With uncontrolled intake of salt over time, the damage
caused by the extra blood pressure may become so severe that
the arteries burst or become completely clogged. This leads
to the death of part of the brain that was receiving the blood
as result of no longer getting oxygen and nutrients it needs
to function. The result is a stroke, where the body loses the
ability to do the things that part of the brain used to control.
Benefits: Common salt, also known as sodium chloride,
is a common ingredient used for seasoning purposes in our
everyday foods. It is available in a range of diverse forms and
particle sizes, depending on the proposed use.
The salt/water ratio is critical for the metabolic rate of our
body. Salt facilitates sending signals in the nerves and muscles
and helps sustain the fluid content inside and outside the blood
cells. Dietary salt exists in various forms: unrefined, refined
(also known as table salt) and iodine-fortified salt. It offers a
variety of health benefits.
Blood pressure and cardiovascular health: It has been
proven that dietary salt determines the blood pressure of
the body and has an impact on cardiovascular health, which
is primarily related to strokes and heart attacks. Inadequate
intake of salts like calcium, magnesium, and sodium can cause
health issues could result in hypotension.
So, Low Blood Pressure (hypotension) (reading below
90/60) can be treated by consuming more salt and hydrating
fluids. This will help boost the volume of blood in the arteries,
resulting in a rise in blood pressure to normal value.
Heat stroke or sun stroke: Heat Stroke is a condition that
occurs when the body’s heat regulating system falls short. This can occur both by being out in the hot sun for a long duration
as well as overheating in the surrounding environment,
such as work areas. The body fails to release heat properly
in order to attain its normal temperature. As a result, the
body temperature becomes too high, which poses a threat to
the major organs. In an attempt to cool itself down, the body
produces more sweat through the sweat glands, thereby losing
essential salt (sodium) and water.
The elderly and small babies are at greater risk of
heat stroke, since their body’s thermostat lacks efficiency.
Prevention of heat or sun stroke is always advisable by keeping
the body hydrated and consuming adequate amounts of salt in
order to maintain the electrolyte balance. A person suffering
from heat stroke can be treated by offering water or fluids that
contain sugar and salt.
Other health benefits of salts include: prevention of goiter
or hyperthyroidism and mental retardation which result from
deficiency of iodine; Oral Rehydration Treatment which is
essential for sustaining the hydration levels of the body-these
electrolytes primarily entail magnesium, potassium, calcium,
and sodium. Also, in diabetes, healthy levels of insulin are
required to maintain a fit body. Diets with low levels of salt can
weaken the body’s sensitivity towards insulin. This reduces
the body’s ability to metabolize glucose, providing poor levels
of energy to the liver, muscles, and nervous system, possibly
leading to Type 2 diabetes.
To maintain a healthy blood pressure and smooth
functioning of the nerves and muscles, the body needs an
adequate amount of salt (sodium). When this optimum level
of sodium falls, water enters into the cells to compensate.
This results in an imbalance of water to salt ratio in the body,
causing swelling in the cells because of excess water.
Interaction, risk, and benefits: An emerging but
inconclusive body of evidence suggests that increased
intake of added sugars might raise blood pressure [11,12].
Studies include animal studies in which rats were fed high
doses of fructose, acute ingestion studies in which humans
were fed high doses of different sugars, and more recently,
epidemiological studies, such as the Framingham Heart Study,
in which consumption of ≥1 soft drink per day significantly
increased the odds of developing high blood pressure [13].
Nonetheless, results from studies in humans are inconsistent,
[14,15] and the chronic effects of a high intake of simple sugars
on blood pressure remain uncertain.
How sugar specifically interact with blood pressure
(Hypertension): The fact is that an underlying cause of high
blood pressure is often related to production of too much
insulin and leptin in response to a high-carbohydrate and
processed food diet. As insulin and leptin levels rise, it causes blood pressure to increase. Eventually, there may become
insulin and/or leptin resistant.
The physiology behind it is that insulin stores magnesium,
but if its receptors are blunted and the cells grow resistant to
insulin, the body can’t store magnesium, so it passes out of the
body through urination. Magnesium stored in the cells relaxes
muscles.
If magnesium level is too low, the smooth muscle of the
blood vessels will be unable to fully relax, and this constriction
raises blood pressure. Fructose also elevates uric acid, which
drives up blood pressure by inhibiting the nitric oxide in the
blood vessels (Uric acid is a byproduct of fructose metabolism;
in fact, fructose typically generates uric acid within minutes
of ingestion).
Nitric oxide helps blood vessels maintain their elasticity, so
nitric oxide suppression leads to increases in blood pressure.
So any program adapted to address high blood pressure
needs to help normalize both insulin/leptin sensitivity and
uric acid level. Eliminating excess sugar/fructose from diet
has incidentally been found to address all these three issues
(insulin, leptin, and uric acid) in one fell swoop.
High intake of salt raises the amount of sodium in the
bloodstream thereby distorting the delicate balance of sodium
and potassium in the body which the kidney uses to pull water
across cell wall from bloodstream into collecting channel
that leads to the bladder. This causes fluid retention which
increases the pressure exerted by the blood against blood
vessel walls, described as high blood pressure (hypertension).
A large number of studies have been conducted which
have consistently shown that salt intake is the major factor
increasing population blood pressure. The evidence is greater
for the effect of salt on blood pressure than any other dietary
and lifestyle factors including a low consumption of fruit and
vegetables (i.e. low potassium intake), obesity, excess alcohol
intake and lack of physical exercise [16].
Two studies [17,18] both 4 weeks in duration, have
compared the effect of different salt intakes on blood pressure
[9,19] and 12g/day in one, [19,20] and 8g/day in the other).
Both showed a clear dose-response relationship, i.e. the lower
the salt intake achieved, the lower the blood pressure.
Also, high intake of sugar raises insulin and leptin levels
in the blood, sometimes leading to insulin and/or leptin
resistance. Insulin stores magnesium, but if the cell receptors
are blunted and the cells grow resistant to insulin, the body
can’t store magnesium, so it passes out of the body through
urination. Magnesium stored in the cells relaxes muscles. If
magnesium level is too low, the smooth muscle of the blood
vessels will be unable to fully relax, and this constriction raises blood pressure (hypertension). Fructose also elevates
uric acid, which drives up blood pressure by inhibiting the
nitric oxide in the blood vessels Uric acid is a byproduct of
fructose metabolism.
The risks associated with high intake of salt and sugar
do not precludes that salts and sugar should be completely
avoided in our diets, as they also have their benefits as stated
earlier in the article. The watch here should be moderation.
Intake of the two should therefore be guided by
recommended amount as proffered experts.
Experts have said that for every 4 gram of salt reduction
from average daily intake, there would be approximately 16%
reduction in deaths from strokes, and 12% reduction in deaths
from coronary heart disease, in any population. Reducing salt
therefore is one of the quickest ways to reduce blood pressure,
particularly if the high blood pressure already exists [21,22].
It is estimated that a reduction of salt by 6g/d would lower
blood pressure by 7/4mmHg in individuals with high blood
pressure and 4/2mmHg in those with normal blood pressure
[21]. The relationships seen in these studies provide evidence
that the recommendation to reduce salt intake to 5-6g/day will
have a major impact on blood pressure and a further reduction
to 3-4d/day will have a much greater effect.
People with or considered at risk of high blood pressure
should take extra care to ensure that they keep their salt intake
below the recommended maximum of 6g. This can be achieved
by simple changes, such as consuming less processed foods and
checking product labels before purchase. Experts recommend
no more than 6 grams of dietary salt (i.e. 2.5 grams of sodium)
on a daily basis. This makes it approx. 1 teaspoon of salt per
day. A good amount of that (about 75%) is already present in
processed meals, breakfast cereals, and breads. Babies less
than one year should not consume more than 1 gram of salt,
whereas the recommended intake for young children changes
as they grow bigger.
As a standard recommendation, total sugar consumption
per day should be kept below 37.5g per day for men and below
25g per day for women [23]. An insulin resistant patient with
high blood pressure, diabetes, heart disease, or other chronic
disease, is advised to limit fructose to 15 grams or less per day,
until condition has normalized [24,25].
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment