Conventional Median Sternotomy vs. Upper Partial Sternotomy in Mitral Valve Replacement-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Background: Full median sternotomy
has been a standard surgical approach for heart surgery for more than 50
years. Several advantages increasing the use of less invasive
approaches to the mitral valve surgery including, cosmetic, blood
product use, respiratory, and pain advantages over conventional surgery.
Parasternal incision, right mini-thoracotomy and partial sternotomy are
described approaches for less invasive cardiac surgery.
Objective: Comparing the standard approach via conventional median sternotomy vs. less invasive approach via upper partial sternotomy.
Methods: Sixty patients, underwent
mitral valve replacement with or without tricuspid valve repair in NHI,
were enrolled in this study and divided into two equal groups, Group I
via conventional median sternotomy (CMS), and Group II via upper partial
sternotomy (UPS). The preoperative characteristics, operative
variables, mortality, and morbidity were analyzed prospectively.
Results:. No difference was found
between the two groups as regards the mortality. However, in Group I,
blood loss was significantly higher, while in Group II cross clamp time
and total bypass time were significantly higher. Minimal invasive group
showed less time on mechanical ventilation, ICU stay and total hospital
stay. In Group I, two patients (7%) developed deep sternal wound
infection, and one patient (3%) suffered unstable sternum. In Group II,
one patient (3%) required conversion to full sternotomy, and one patient
(3%) required permanent pacemaker.
Conclusion: Upper partial sternotomy
considered a safe alternative for mitral valve replacement; it provides
adequate exposure for valve. Conventional cardiopulmonary bypass and
cardioplegia solution administration can be used, as no specific
instruments or endoscope were need, and superior on conventional
technique as provided better patient satisfaction for pain and cosmetic
outcome.
Introduction
In the mid-1990s, minimally invasive approaches for
mitral valve operations were pioneered with the intent of reducing
morbidity, postoperative pain, and blood loss; improving cosmesis;
shortening hospital stay; and reducing cost compared with the
50-year-old conventional median sternotomy approach. Furthermore, it was
believed that less spreading of the incision, no interference with the
diaphragm, and less tissue dissection might improve outcomes,
particularly respiratory function [1,2].
Indeed, a less invasive approach to cardiac surgery
has been widely adopted in clinical practice [3,4]. Compared to
conventional full median sternotomy, less invasive approaches
reduce incision size and surgical trauma. It has been reported to reduce
morbidity, accelerate recovery, and shorten hospital [3,5], with
equally durable late outcome [6]. Several incisions for minimally
invasive cardiac surgery has been described: parasternal incision [7,8]
right mini-thoracotomy [9-11] & partial sternotomy [12-14].
from August 1, 2015 till the end of September 30,
2016, Sixty patients were prospectively enrolled in our study and
randomly assigned into two equal groups, group I conventional median
sternotomy (CMS group, n=30) or group II upper partial sternotomy (UPS
group, n=30). All patients were operated bythe same surgeon. The study
was done in the national heart
institute (NHI).
Group I CMS incision was 25 to 30cm long. It began 1 to
2cm below the sternal notch and extending downwards to
the xiphoid process. The full sternotomy was performed from
sternal notch and extended downwards to the xiphoid process.
Cannulation: Central arterial cannulation of the ascending
aorta and venous cannulation of superior and inferior vena
cavae. Mitral valve exposure through stander paraseptal left
atriotomy. Tricuspid valve exposure through right atriotomy,
and tricuspid repair was done by de-vaga on beating heart if
needed.
Group II UPS incision was 8 to 10cm long. It began half
way between the sternal notch and the angle of Louis, and
ended above the fourth intercostal space. The upper partial
sternotomy was performed from sternal notch and extended
to the left fourth intercostal space, forming a reverse j-shape
sternotomy. Care was taken not to injure the left internal
thoracic artery. Cannulation: central arterial cannulation of the
ascending aorta and superior vena cava before establishing thebypass and inferior vena cava was cannulated after initiation
of the bypass on an empty heart. Mitral valve exposure through
transseptal approach. Tricuspid valve exposure through same
right atriotomy incision for the transseptal approach and
tricuspid repair were done same as group I.
Conventional general anesthesia, standard cardio
pulmonary bypass, and myocardial protection using
intermittent perfusion of ante grade warm blood cardioplegia
into the aortic root were conducted in both groups.
All data were collected on standardized forms, entered
in a computerized database, and analyzed with statistical
software. Results were statistically represented in terms of
range, mean, standard deviation and percentages. Continuous
data of different groups were compared with paired t-tests
and categorical data (parametric data) by Pearson’s chisquare
x2 test was performed. A p value <0.05 was considered
statistically significant.
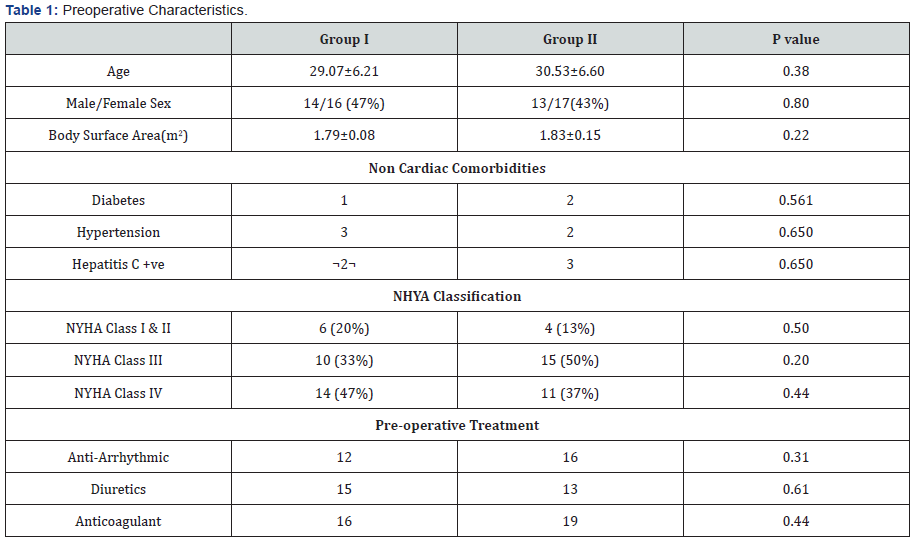
There were no statistically significant differences
between Group I and Group II as regards to the preoperative
characteristics. Patient’s preoperative Characteristics were
shown in Table 1.
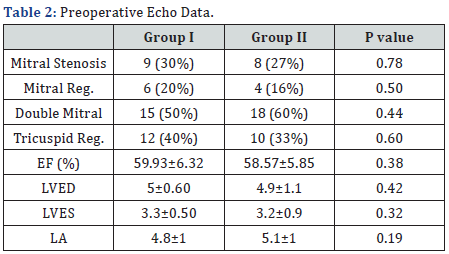
There were no statistically significant differences between
Group I and Group II as regards to the patient’s preoperative
echo data as shown in Table 2.
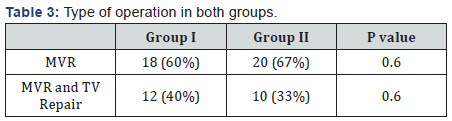
There were no statistically significant differences between
Group I and Group II as regards to the type of operation as
shown in Table 3.
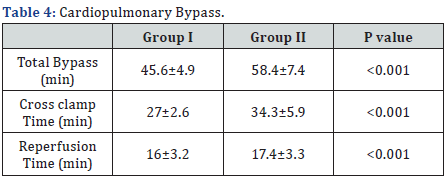
There were statistically significant difference between
Group I and Group II as regards to the total bypass, cross clamp
and consequently the reperfusion time, all were significantly
longer in group II, as shown in Table 4.
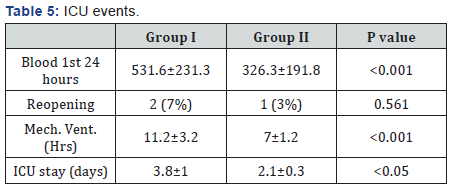
In Group I, blood loss was significantly higher, while in
Group II time on mechanical ventilation and ICU stay were
significantly less, and there was no significant difference for
reopening for bleeding, as shown in Table 5.
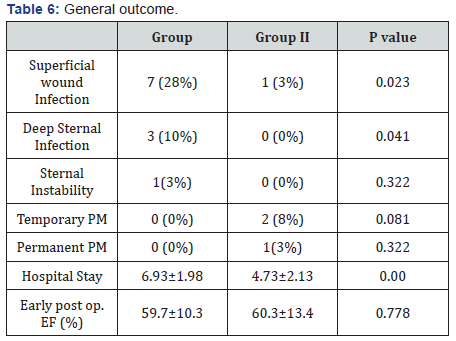
In Group I, superficial wound infection was significantly
higher, while in Group II total hospital stay was significantly
less. There were no statistically significant difference between
Group I and Group II as regards to deep wound infection,
sternum instability, the need of temporary or permanent
pacemaker and finally the ejection fraction at time of discharge,
as shown in Table 6.
In our study we considered the partial or mini sternotomy
in Group II as a less invasive cardiac approach, however
our study was not concerning with the mini thoracotomy
approach, we determined adequate familiar working field with
appropriate exposure of mitral valve through a smaller limited
incision, which appear to be pretty different in comparison to
thoracotomies exposure for cardiac procedure. McClure et al.
[6] reported certain degree of variation from patient to patient
regarding the relation between the different structures of the
heart and the chest wall which is not significant for the surgeon
when using large incisions. While with smaller incisions the
preference is for the ministernotomy incision [15]. While in
mini sternotomy, Hsiao et al. [5] reported that this incision
affords the surgeon a familiar operative field from which
either mitral valve repair or replacement are possible.
In our study all patients were lying in supine, no special
position is required for the UPS group. Lehr et al. [11] reported
that in minimal invasive mitral valve through minithoractomy,
the patient is placed on the operating table in supine position,
with the right hemithorax elevated 30 degrees and the hips
flat. While minimal invasive through thoractomy partial
sternotomy were reported lying in supine, [5,13,14].
In our study the cardio pulmonary bypass was obtained
in standard approach by central aortic cannulation in both
groups, with no need for peripheral cannulation. Hsiao et al.
[5] reported that central aortic and venous cannulation are
possible and the ascending aorta can be cross-clamped directly,
without the need for endovascular clamping. In contrast with
the thoracotomies. The common femoral artery is the most
common site for perfusion [11].
Serious drawbacks were recognized for that technique:
peripheral atherosclerosis may preclude cannulation,
retrograde dissection or emboli may ensue, and other
complications such as postoperative wound infection,
hematoma, lymphocele, arteriovenous fistula, or stenosis
of the femoral vessels may develop [16]. Wolfe et al. [17]
reported ischemic injury to the leg as a documented potential
complication of femoral arterial cannulation. The proposed
mechanisms for this injury include misidentification of the
common femoral artery, cannulation of a small femoral system,
excessive perfusion times, unidentified vascular disease
within this arterial system, and vascular injury or narrowing
after removal of the cannula.
Half of the patients in this study received less invasive
cardiac surgery via partial sternotomy without endoscopic or
robotic help, in their series, it was possible in certain cases to
carry on simple techniques by watching only the monitor, but
most often the successful repair of the mitral valve required
direct vision. Endoscopic or robotic assistance was not
required [5].
In our study, there was no need to use long-shafted
instruments or a knot-pushing device. There was need for
extra cost for the instruments or devices. Same opinion was
for Chen-Yuan Hsiao et al. [5] they concluded that less invasive
cardiac surgery via partial sternotomy does not need longshafted
instruments or a knot-pushing device. a shorter
learning period can be expected, and additional cost for
specific instruments or devices might not be necessary.
The main impediment to adoption of any new surgical
approach is that it requires the learning of a different
technique, there was a learning curve involved in developing
the technique, which was, however, technically similar to
conventional sternotomy [1]. The surgeon can utilize this
technique with a very short learning period [5].
Were longer in Partial Sternotomy surgery were also
reported in other studies [18,4]. However, Mihaljevic et al.
[20] reported significantly shorter aortic cross-clamping and
cardiopulmonary bypass times in patients undergoing partial
sternotomy. Another opinion was reported by Svensson et al.
[1] the Intraoperative support among the patients, ischemic
time was slightly longer after a minimally invasive approach
(65+/-24 VS 62+/-23minutes, P=0.1), and cardiopulmonary
bypass time was equivalent.
There was only one patient (3%) who underwent conversion
from partial to full sternotomy due to inadequate exposure for
mitral valve. Also Hsiao et al. [5] reported one patient (3%)
who underwent conversion from partial to full sternotomy due
to inadequate exposure for mitral valve replacement. While
Tabata et al. [21] reported that 24 of 907 patients required
conversion from upper partial sternotomy because of bleeding,
ventricular dysfunction, refractory ventricular arrhythmia,
poor exposure, and other causes. Twenty-one of 528 patients
required conversion from lower partial sternotomy; none died
postoperatively. The authors concluded that conversion from
upper sternotomy was associated with serious morbidity and
mortality. Mihaljevic et al. [20] when conversion is necessary,
partial sternotomy can be easily enlarged to full sternotomy.
In our study, the blood loss were reported to be significantly
higher in Conventional Median Sternotomy, The mean blood
loss was 531.6mL (Table 5), Less invasive cardiac surgery
through partial sternotomy has been reported to reduce postoperative
bleeding, and therefore the less blood transfusion.
Many studies support this, outcome [1,15,20,22].
Patients operated on using minimally invasive surgery
present, in general terms, less time on mechanical ventilation
than patients operated on in the conventional way with mean
ventilation time of 7hrs and less ICU stay of 2.1 Days (Table 5).
The majority of authors observe benefits in earlier extubation,
better recovery of respiratory function and the reduction of the
time spent in intensive care and total time in hospital [20,23-
25]. Also Svensson et al. [1] reported A higher proportion of
patients were extubated in the operating room.
There were less incidence of superficial and deep wound
infection and also sternal instability (Table 6), lesser incidence
of infectious complications, with no deep wound infection in
our patients in less invasive cardiac surgery was reported
[4,23,29].
One of the potential advantages in our study is the
cosmetic benefit special for the young females; Brinkman et al.
[29] also reported a cosmetic benefit which is one of the great
advantages of these approaches in the case of young patients.
Also Bonacchi et al. [24] reported that partial sternotomy
provided a better cosmetic result.
In our study, 2 (7%) patient in UPS group need to
temporary pace maker for transient instability and only 1 (3%) patient needed permanent pacing, Table 6. José Navia
[14], reported Four percent of patients required permanent
pacemaker implantation for the postoperative heart block
or bradycardia. Also Cosgrove & Gillinov [13], reported two
percent of patients needed a permanent pacemaker. While
Robert et al. [14] reported four patients had junctional rhythm
in the postoperative period, but this did not persist.
In our study we noticed the postoperative need of
analgesics to be much lesser in the partial sternotomy group,
which reflects the potential benefit of pain reduction. Studies
reported the reduction of pain felt by the patient and the
demand for analgesics in the immediate postoperative period
[15,24,30]. Svensson et al. [1] reported less pain in the first 24
hours after the operation (P<.0001) for minimally invasive
surgery patients had but similar pain scores thereafter with
the conventional. Compared to patients receiving lateral
thoracotomy, less pain was reported in patients undergoing
partial sternotomy [31].
One of the objectives of minimally invasive approaches is to
reduce surgical aggression and thus favor functional recovery,
in ours we found the mean duration of hospitalization was 5.6
(Table 6) in Partial Sternotomy. The benefit of these approaches
in terms of the impact on the duration of hospitalization is
quite uniform, and the majority of authors observe benefits in
the reduction of the average hospital stay [24,25,27,29]. On the
other hand Svensson study does not show differences in the
duration of the hospitalization [1].
In ours there were no mortality in both groups, comparative
studies have demonstrated that there are no differences
in early mortality between minimally invasive approaches
and a complete sternotomy [15], also late outcome Survival
at 5, 10, and 15 years was 93%±1%, 86%±1% and 79%±3%,
respectively (median survival, 15 years; 95% confidence
interval, 14.9-15.4). Freedom from reoperation was 100% for
mitral valve replacement at late follow-up [6].
There are several limitations in our study. The patient
number was limited, and this was a prospective study in one
single hospital. Long term functional status and survival
follow-up are necessary in any future study, also the first
images we can see the cosmetic benefits of the mini-sternotomy
technique, as all cardiac surgeries in this study were the first
for the patients.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment