Contegra Graft in the Surgical Management of Double Outlet Right Ventricle (DORV)-A Case Report-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY &
CARDIOVASCULAR THERAPY
Abstract
DORV is a complex congenital heart disease where both
great vessels arise entirely or predominantly from right ventricle.
This report describes the case of a 10 year old female with DORV. The
cardiac anomalies were corrected with split Dacron patch for VSD and
contegra conduit graft for reconstruction of right ventricular outflow
tract. She showed excellent postoperative outcome and was discharged
with advice to be on a regular follow up.
Abbreviations: RVOT: Right Ventricular Outflow Tract; DORV: Double Outflow Right Ventricle
Introduction
The spectrum of DORV is complex, heterogeneous and
varies between Tetralogy of Fallots (TOF) at one end and complete
Transposition of great arteries (TGA) at the other end and surgical
correction also varies according to the complexity of the situation ⦋1⦌.
When more than 50% of the great arteries arise from right ventricle, it
is accepted as DORV. The DORV may be of four subtypes:
- Subaortic.
- Subpumonary.
- Doubly committed.
- Non-committed, according to the relationship of the Ventricular septal defect (VSD) to the great arteries ⦋2⦌.
The definitive management of DORV is always surgical.
The contegra grafts are derived from bovine internal jugular vein with
its trileaflet venous valve, preserved in buffered glutaraldehyde
solution, available as 10-22mm size, are readily available from shelf
for right ventricular outflow tract (RVOT) reconstruction where
homografts or composite pulmonary conduits fail or are not easily
available ⦋3⦌ (Figure 1).

A 10-year-old girl was admitted into cardiac surgery
department of BSMMU, with central and peripheral cyanosis since 7-8
months of her birth and gradually worsening shortness of breath on
exertion in last few months. On admission she was 133cm in height, 24kg
in weight and her pulse rate was 114 beats per minute, respiration rate
was 24/min, blood pressure was100/50mm of Hg. She had finger and toe
clubbing, moderately bulged out precordium, systolic thrill and murmurin
the pulmonary area. Chest x-ray revealed typical boot-shaped
heart, EKG showed obvious right ventricular hypertrophy, color
Doppler echocardiography showed 16mm subaortic VSD with
predominantly right to left shunt, with more 50% overriding of
aorta, with severe infundibular, valvular and main pulmonary
stenosis having transvalvular peak pressure gradient more than
105mm of Hg, but having left ventricular ejection fraction of 71%.
MDCT revealed the sizes of main pulmonary artery (8mm), right
pulmonary artery (10.7mm), left pulmonary artery (16.4mm)
respectively, the main pulmonary artery was less than 25% of
the aorta, pulmonary valve was very narrow with fibrosis and
speckles of calcification. Major aortopulmonary collaterals were
absent however. Cardiac catheterization was not done, because
we thought it redundant (Figure 2).
Procedure Details
The patient was operated on 19 January, 2015. Under
general anesthesia with endotracheal intubation and broad
spectrum antibiotic coverage, standard median sternotomy and
pericardiotomy was done to expose the heart. Cardiopulmonary
bypass was established with bicaval cannulation and aortic
cannulation. Heart was arrested with aortic root antegrade
cardioplegia and mild hypothermia (32 ˚C) after application
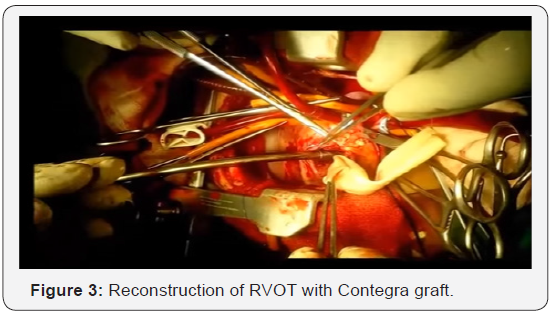
of cross-clamp. The subarterial VSD was approached through
right vetriculotomy, RVOT muscle bands were resected, VSD was
enlarged anteriorly and was repaired by a split-opened Dacron
tube graft to produce intracardiac buffle, it reduced the right
ventricular cavity size. The severely stenosed main pulmonary
artery was resected, proximal end was closed with double layered prolene suture, the right ventriculotomy was anastomed
obliquely to the proximal end of Contegra graft (20mm) which
enlarged the right ventricular cavity to some extent, the distal
end of the graft was anastomosed to split-opened, enlarged
distal pulmonary artery. The weaning from bypass, recovery in
the ICU were uneventful (Figure 3).
The patient was advised to take Aspirin 75mg daily and
was discharged home after 14 days. Follow-up at 1 month,
3 months, 6 months revealed well-functioning graft with
an acceptablegradient (25-35mm Hg). However from 9
monthsonward, there is a tendency of increasing gradient, at
present, it is 45-50mm of Hg, but the patient is asymptomatic.
We have kept her on low diuretics, low-dose propranolol, and
ambrisentan. We will follow her up regularly to see the longterm
patency of the graft and timing of a second look operation.
Double outlet right ventricle (DORV) refers to family of
anatomically related complex congenital cardiac lesions involving
the outflow tracts. The selection of the operative technique
depends on the VSD’s position and its relationship to the great
arteries ⦋4⦌. We reconstructed the RVOT with contegra graft and
VSD with Dacron patch to produce the intracardiac baffle. The
contegra valved heterograft conduit has emerged as a reliable
alternative for the reconstruction of right ventricular outflow
tract. Contegra conduit device was granted as humanitarian use
device in 2002 and approved to profit on the sale of contegra in the
year 2013 ⦋3⦌. Availability of different sizes, suitable alternative
to cryopreserved homografts, easy to perform reconstructive
procedure due to adequate length and moderate costs make it as
a good alternative. Moreover, early postoperative and mid-term
results have been satisfactory ⦋5⦌. One study reported 96% rate
of survival at 5 years and 10 years respectively, freedom from
re-intervention 65.2% at 10 years, freedom from endocarditis
94.4% at 5 years and 10 years interval, pulmonary insufficiency/
stenosis in 38.5% during mean follow-up of 10 months. Similarly,
pressure gradient ≥50mm Hg was 79.9% at 5 years and 63.5% at
10 years respectively ⦋6⦌.
The surgical treatment of DORV is complex and challenging.
Our experience of using contegra conduit graft for the
reconstruction of RVOT has shown excellent outcome. It may
be the treatment of choice for complex congenital heart disease
in need of RVOT reconstruction. Extensive clinical trials are
needed to understand the efficacy of contegra conduit graft
as a treatment of choice for RVOT reconstruction in complex
congenital heart disease.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment