Vessel Architecture and Excessive Coronary Artery Instrumentation as a Cause of Coronary Artery Perforation-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Coronary artery perforation (CP) is a rare but
catastrophic complication of percutaneous coronary intervention (PCI).
Grade three coronary artery perforation and rupture results in
pericardial effusion and tamponade requiring urgent pericardiocentesis.
Advances in coronary intervention have increased the opportunity to
treat coronary artery perforation. We report a case of an elderly male
patient with multiple cardiovascular risk factors presenting with Non-ST
Elevation Myocardial Infarction (NSTEMI) complicated with pulmonary
edema. Coronary angiogram (CAG) revealed severe triple vessel coronary
artery disease (CAD) with heavy calcifications. Successful
recanalization of mid left anterior descending coronary artery (LAD)
chronic total occlusion (CTO) with heavy and floppy guidewires followed
by stepwise rotational atherectomy (RA) with two different sizes burrs
and high pressure balloon (HPB) dilation then deploying three
drug-eluting stents to proximal to very distal (LAD), with post-dilation
with (HPB) then deploying drug-eluting stent to tortuous proximal to
mid left circumflex. After PCI, Grade three coronary artery perforations
was noted at the stented mid to distal (LAD) acute cardiac tamponade
developed to which emergent prolonged balloon inflation, reversal of
anticoagulation and pericardiocentesis were done, covered stents were
deployed.
Introduction
Coronary artery perforation (CP) is a rare but
catastrophic complication of percutaneous coronary intervention (PCI).
Perforation occurs in 0.1% to 3% of cases with mortality rates
approximately 10%. Grade III coronary perforation and rupture results in
pericardial effusion and tamponade requiring urgent pericardiocentesis
in up to 60% of cases [1]. Advances in coronary intervention have
increased the opportunity to treat coronary artery perforation. We
report a case of 87 years old male with multiple cardiovascular risk
factors who presented with non-ST segment elevation myocardial
infarction (NSTEMI) complicated by pulmonary edema. Coronary angiogram
(CAG) revealed severe triple vessel coronary artery disease (CAD) with
heavy calcifications of the left main coronary artery and its branches.
During (PCI), he had Ellis type III coronary artery perforation, cardiac
tamponade and shock. The patient was supported with inotropes and
intra-aortic balloon pump (IABP), prolonged balloon inflation was done,
pericardiocentesis was done, and covered stents were deployed.
The patient was 87 years old male with a history of
hypertension, type two diabetes mellitus presenting with shortness of
breath progressively ending into respiratory distress over two days
before admission to our department, the patient had a history of chronic
kidney disease stage 3, serum creatinine was 1.68mg/dl on admission
which became 2.23mg/dL thereafter, and positive Toponin I at admission,
electrocardiogram showed sinus tachycardia with minimal ST depression at
inferolateral leads, minimal ST segment elevation at V1-V4 with
pathological Q waves, chest x-ray showed pulmonary edema, under
impression of NSTEMI he was admitted and scheduled for an angiogram
which showed severe triple vessel coronary artery disease with heavy
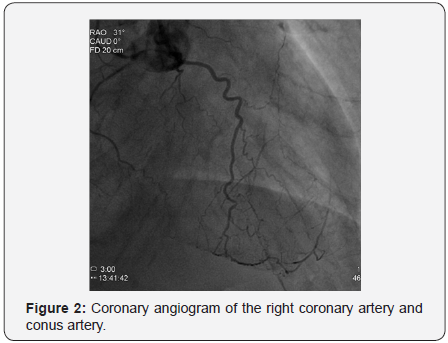
calcifications of left system as illustrated in Figures 1 & 2; the
proximal left anterior descending artery (LAD) had severe stenosis 93%,
the mid left anterior descending artery (LAD) had chronic total
occlusion (CTO) after giving a large septal branch and second diagonal
(D2), collaterals to CTO segment from distal left circumflex
artery (LCx) Grade 1/3; p-LAD bridging collaterals Grade 1/3
and large epicardial tortuous collateral from conus branch to
distal LAD Grade 3/3, the proximal left circumflex artery (LCx)
was acutely angled tortuous vessel with heavy calcifications
showing proximal stenosis 74%, and the right coronary artery
(RCA) was small non-dominant diffusely diseased vessel (Syntax
score: 39.5), Echocardiogram showed borderline left ventricular
performance with resting wall motion abnormalities, dyspnea
then progressed, and acute respiratory distress developed that
necessitated respiratory support with mechanical ventilation
and hemodynamic support with intra-aortic balloon pump
(IABP).

In order to perform (PCI) left trans-radial (TR) access
was established then with the use of sheath-less technique
seven French system (7F EBU4) (Launcher Medtronic) guiding
catheter (GC) was used to engage the left main coronary artery
(LMCA). A 0.014 Fielder FC guidewire (GW) was loaded on
single lumen micro-catheter (MC) and was used to re-canalize
CTO from mid LAD. After failure to do so using two Fielder FC
guidewires, we switched to a Fielder XT-A guidewire which was successful to pass to the severely calcified mid to distal LAD
with ante-grade approach. With anchoring balloon technique a
2.0x20mm Mini-Trek balloon at D2 branch at 12 atmospheric
pressure unites (atm), we inflated a 1.2x6mm Mini-Trek(Abbott
Vascular) balloon at 16-20atm at the CTO cap, then 2.0x20 Mini-
Trek balloon at mid to distal LAD at 18-20 atm. Long dissection
from very distal LAD was noted. To facilitate delivery of stents
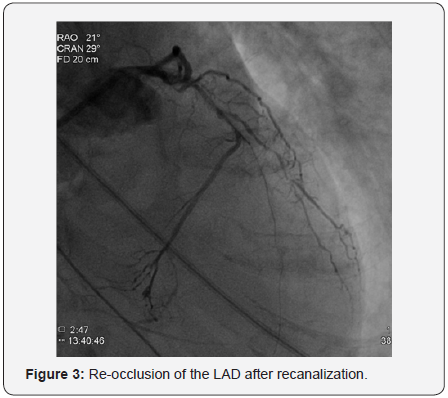
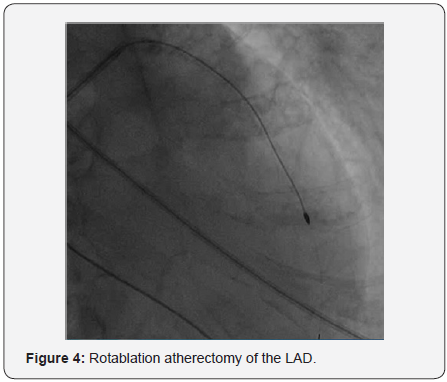
a 0.009” Rota Wire was substituted for Fielder FC to very distal
LAD and rotational atherectomy (RA) de-bulking was done in a
stepwise manner with 1.25 mm, then 1.5 mm burr at 180K-220K
rpm as illustrated in Figures 3 & 4. We dilated the whole LAD
with 2.0x20mm Mini-Trek at 20 atm then 2.5x15mm Hiryu
(TERUMO) high pressure balloon (HBP) at 28 atm at proximal
to mid LAD, then 3.0x15mm Hiryu HPB was inflated at p-m-
LAD at 24-26 atm in order to facilitate stent passage through
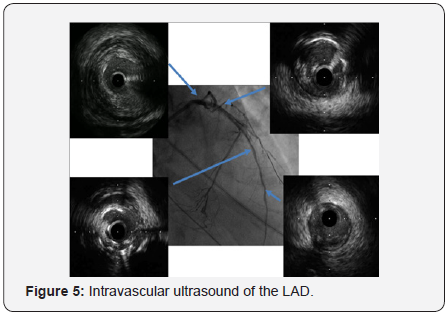
calcified mid LAD, subsequently we interrogated the LAD with
intravascular ultrasound (IVUS) as illustrated at Figure 5.
Three drug eluting stents (DES) everolimus eluting stents
(EES) Xience Prime 2.25x28mm, 2.75x38mm, and 3.0x38mm
(Abbott Vascular) were deployed from very distal to proximal
LAD at 7-10atm, and followed by post-dilation with a 3.0x15 mm
Hiryu (TERUMO) HPB at mid to proximal LAD at 20-24atm. A
new Fielder FC GW was loaded on a second new Fine-cross MC
and was advanced to distal LCx in order to treat the proximal
LCx stenosis. With anchoring a 3.0x15mm Hiryu (TERUMO)
HPB at mid LAD at 20atm, a 1.2x6mm Mini-Trek balloon (Abbott
Vascular) was passed through acute-angled proximal to mid LCx,
then inflated at mid LCx at 20atm, then further dilatation with
2.0x12mm Mini-Trek balloon (Abbott Vascular) at 20atm and
2.5x15mm Hiryu (TERUMO) HPB at 26atm.
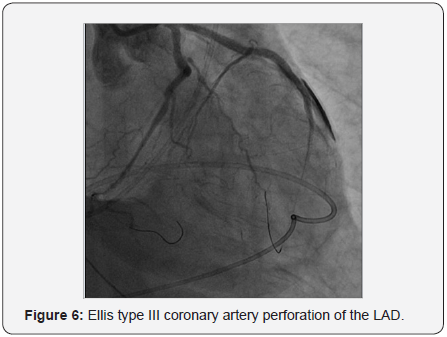
Ellis type III perforation from stented mid to distal LAD
was noted as illustrated in Figure 6. Initially we used balloon
inflation at the perforation site to seal the leakage. Bedside 2
Dimensional echocardiography showed acute cardiac tamponade
with surrounding effusion of more than 100cc. Emergent
pericardocentesis was done via subcostal approach with systolic
blood pressure restored to more than 100mmHg after draining
bloody effusion (250cc) from pig-tail catheter. Protamine 50mg
was administered. We completed deployment of a 2.75x33mm
(EES) Xience Prime DES (Abbott Vascular) at proximal to mid LCx under 5.5F guide-liner catheter support and anchoring a
3.0x15mm Hiryu (TERUMO) HPB at mid LAD at 24atm.
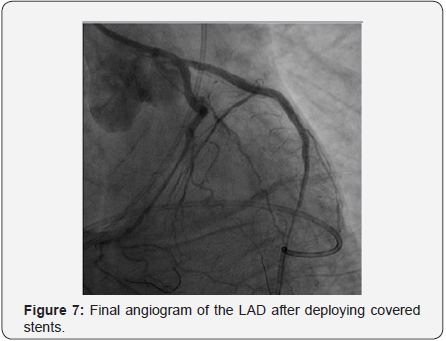
A 2.8x19mm polytetrafluoroethylene (PTFE) covered stent
Graft-master stent (Abbott Vascular) was placed at mid to distal
LAD at 16 atm followed by post-dilatation with 3.0x15mm Hiryu
(TERUMO) HPB at 26 atm. Persistent dye extravasation was
noted. Another 2.8x16mm Graft-master covered stent was placed
at distal LAD overlapped the last one, sealing the perforation site
as illustrated in Figure 7. The patient gradually improved under
ventilator & IABP support.
Percutaneous coronary intervention has become a leading
therapeutic treatment option for coronary artery disease,
especially in the setting of ACS [2]. Chronic total occlusions (CTO)
remain the most challenging lesion subset in percutaneous
coronary interventions (PCI). This is due to the suboptimal
visualization of the vessel distal to the occlusion (exclusively
through collaterals) and the adverse anatomical characteristics
of the plaque, which is usually resistant to wire manipulation
due to fibrotic and calcific components. Conventional CTO
wiring techniques (antegrade “true-to-true lumen” approach)
have traditionally been associated with low success rates (60-
80%) and higher incidence of complications, as compared with
non-CTO intervention [3], modern practice have shown more
wide adoption of sub-adventitial techniques for CTO PCI.
In our case here patient related risk factors for CP where,
hypertension, elderly age, chronic renal insufficiency, coronary
artery calcification, tortuosity, and type C lesions, while
procedure related risks include the use of hydrophilic wires, IVUS
and Rotational atherecromy, and high pressure balloon inflation
either for post-dilation or for anchoring. In a metanalysis of 16
studies by Shimony et al. [4] involving 197, 061 PCIs, the pooled
incidence of CP was 0.43% (95% CI 0.35-0.52%) [4].
According to Al-Lamee et al. [2] study of the incidence and
the outcome for grade III CP, the commonest cause was inflation of an intracoronary balloon, with no change in the incidence
based on the balloon compliance. Grade III CP was caused
by rotablation, directional atherectomy, and cutting balloon
inflation in only a small number of cases [2].
In a cohort conducted by Barnett et al. [1] the acute and
up to 12 month outcome of 6031 PCI from 2005 through 2011,
patients who received PFTE covered stents were followed to
evaluate the incidence of major cardiac events. Major cardiac
events were defined as: cardiac tamponade, death, emergent
surgical drainage, myocardial infarction, or the need for
emergent coronary artery bypass grafting, PFTE graft stent
placement for coronary artery perforation during PCI was found
to be beneficial acutely and up to 12 months following PFTE
placement [5].
In 2005, Colombo et al. [6] suggested an approach for the
recanalization of occluded coronary arteries, which was termed
“Subintimal Tracking and Re-entry” (STAR technique). STAR
demonstrated that dissecting through the sub-adventitial space
could traverse long occlusion segments safely and rapidly,
increasing operators’ confidence in traversing this blind end
segment. Briefly, STAR creates a sub-adventitial cleavage
plane by advancing a hydrophilic coronary wire with a J-loop
configuration at its tip (“knuckle”) to allow a blunt dissection
between the anatomical planes of the vessel, with the aim to
re-enter into the true lumen distal to the occlusion. Initial
experience with STAR was encouraging, with final thrombolysis
in myocardial infarction (TIMI) 3 flow achieved in 97% of
cases, and full recanalization of the main vessel and most distal
branches in 67%. Coronary artery perforations were observed
in 10% of patients. Five-month follow-up showed restenosis
rates of (52%), initially attributed to the use of bare-metal
stents (BMS), first-generation drug-eluting stents (DES), and
long stented segments [6]. TIMI flow grade <3 following stenting
independently predicted restenosis [7].
CTO PCI has been associated with a variety of complications
of these CP is the most feared and dramatic life-threatening complication. All operators, assistants and technicians should be
prepared with required skills, technology and tools to avoid and
manage such catastrophic complication. The use PTFE covered
stents is considered the most optimal available therapeutic
option for acute management of CP especially with unfavorable
hemodynamics and persistent leakage.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php
To know more about Juniper Publishers please
click on: https://juniperpublishers.business.site/



Comments
Post a Comment