Sudden Intraventricular Conduction System Defect Prior to Urgent Coronary Artery Revascularization-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Intraventricular conduction abnormalities have been
thoroughly described in the setting of post cardiac surgery in
particular after valvular surgery. It’s also widely known that several
anaesthetic factors are known to cause autonomic disturbances resulting
in unmasking of a sinus node dysfunction, significant bradycardia, and
cardiovascular collapse during the intraoperative period. However,
little is known on asymptomatic episodes in particular prior to CABG. We
report a rare occurrence of intraventricular conduction defect that
presented in an asymptomatic patient following NSTEMI and prior to
urgent coronary artery revascularization. We aim to highlight the
measures that were taken to manage this.
Keywords: Conduction defect; Sick-sinus syndrome; Coronary revascularization
Abbrevations: NSTEMI: Non-ST
Elevation Myocardial Infarction; ECG: Electrocardiogram; LCM: Left Main
Stem; LAD: Left Anterior Descending Artery LCx: Left Circumflex RCA:
Right Coronary Artery; CABG: Coronary Artery Bypass Grafting Surgery;
AV: Atrioventricular CPB: Cardiopulmonary Bypass; LIMA: Left Internal
Mammary Artery SVG: Saphenous Venous Graft; PDA: Posterior Descending
Artery; AF: Atrial Fibrillation; TED: Transoesophageal Echocardiography;
PPM: Permanent Pacemaker; VCD: Ventricular Conduction Defects
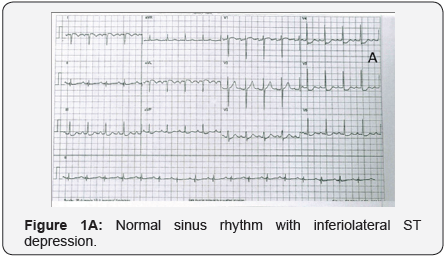
We report a 61-year-oldmale, who was admitted to our
centre with sudden onset of chest pain. He was diagnosed with non-ST
elevation myocardial infarction (NSTEMI). His electrocardiogram (ECG)
showed normal sinus rhythm with inferiolateral ST segment depression
(Figure 1A). Patients past medical history include ex-smoker, controlled
hypertension, non-insulin dependent diabetes mellitus, peripheral
vascular disease, hypercholesterolemia, iron deficiency anaemia and
Hepatitis B.
The patient’s immediate angiogram revealed a right
dominant heart with severe distal left main stem (LMS) disease which was
80% occluded. The left anterior descending artery (LAD) was diffusely
irregular with severe mid-vessel disease. It was noted that the patient
had a high diagonal artery with severely diseased proximal portion. The
left circumflex (LCx) artery territory was with mild irregularities and
severe diffuse disease. The right coronary artery (RCA) was diffusely
diseased.
Patients’ condition was optimized and stabilized
medically. Due to diffuse multi-vessel involvement, the patient was
deemed suitable for in-patient coronary artery bypass grafting surgery
(CABG).
Seven days following his presentation, the patient
underwent surgery. On induction of anaesthesia, whilst inserting the
central venous line into right internal jugular vein, the patient
develop edacute episode of sinus tachycardia followed by sinus
bradycardia of 40 beats per minute. A bolus dose of 5mcg of adrenaline
was given to maintain his heart rate. Preliminary impression was that
patient must have sustained an infraction entailing the atrioventricular
(AV) conduction system. Cardiopulmonary bypass (CPB) was instituted
immediately and
patient’s status was stabilized.
He underwent CABG utilizing left internal mammary artery
(LIMA) to LAD and saphenous venous graft (SVG) to obtuse
marginal and posterior descending artery (PDA). The CPB
time was 77mins and aortic cross clamp time was 35mins. The
patient was weaned off CPB support in sinus bradycardia. Two
epicardial pacing wires were placed and patient was externally
paced.
Three days following his CABG, patient became haemo
dynamically unstable with alternate episodes of tachy-brady
arrhythmias concomitant with atrial fibrillation (AF). For rate
control, the patient was loaded with intravenous amiodarone.
His status necessitated neither inotropic support with nor
adrenaline to maintain adequate blood pressure and urine
output.
Bedside transoesophageal echocardiography (TOE) was
performed to exclude cardiac tamponade; the findings from the
TOE were unequivocal with no presence of left atrial thrombus.
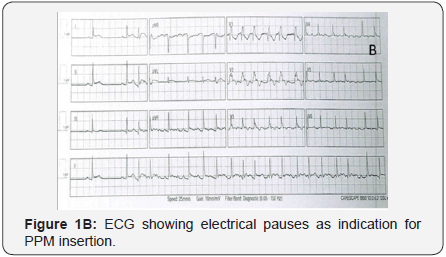
Subsequently, an urgent consultation with our local
electrophysiology team was sought for. It was noted that the
tachy-brady arrhythmias included multiple electrical pauses
(Figure 1B) alternating with atrial fibrillation. The decision
was made to insert a dual chamber permanent pacemaker
(PPM). Following insertion of PPM, the patient was persistently
sustaining intermittent rapid ventricular rate AF episodes and
he was given oral beta-blocker. Following to this the patient’s
heart rate was controlled and he was eventually discharged to
the ward.
Electrical conduction abnormalities are well-recognized
complications of acute myocardial infarction [1]. They are caused
by either autonomic imbalance or ischemia and necrosis of the
conduction system. The most common clinical consequence is
bradycardia, which may or may not be symptomatic. Complete
heart block with a slow escape rhythm is a potentially fatal event
in this setting if not detected and treated promptly.
Anaesthesia related autonomic imbalance may unveil an
undiagnosed sick sinus syndrome [2]. However, in diagnosed, asymptomatic patients one would contemplate preoperative
insertion of a temporary pacemaker prior to anaesthetic
induction as the latter had clearly been described altogether
with surgical manoeuvres to induce an autonomic misbalance
leading to serious dysrhythmias resistant to conventional
pharmacological treatment.
Preoperative, intra operative and postoperative variables,
which might play a role in the development of ventricular
conduction defects (VCD) and atrial fibrillation (AF) following
coronary artery bypass grafting (CABG), were previously
described in the literature. Caretta et al. [3] evaluated 236
consecutive patients who sustained VCD and AF postoperatively
and reported an incidence of 15.5% amongst their patients’
cohort. In their analysis, they demonstrated that left main disease
and right coronary artery occlusion associated with significant
stenosis of the proximal left anterior descending artery were
amongst the potential factor that could lead to conduction
abnormalities. It also notable to mention that they reported on
the duration of aortic cross-clamp time which was contributory
factor to the development of conduction abnormalities and
sequelae.
Compounded by these risks, it’s quite common to practicing
cardiac surgeons the knowledge of development of postoperative
AF following cardiac surgery [4] and the link between ischaemic
injuries, with increasing duration of cardioplegic arrest, seems
to play a key role in such incidence. Yet, non homogeneous
cardioplegic delivery to critical areas of myocardium, and
particularly to the specialized conducting system, may cause
VCD after CABG.
Passman et al. [5] described a model where by the incidence
of AF post cardiac surgery could potentially be quantified
and predicted. They describe the occurrence of conduction
abnormalities to be related to advanced age >65 years, PR
interval >/=180 milliseconds and a P-wave duration in lead V1
>/=110milliseconds. Such peculiarities could potentially lead to
prevention protocols to avert patients from sustaining AF post
cardiac surgery which has long health and cost implications.
However, in this case report, we demonstrated that intra
ventricular conduction defect and abnormalities occurred
essentially at induction of anaesthesia in otherwise normal
and asymptomatic patient with normal sinus preoperative ECG
rhythm. Although bradycardia associated with vecuronium,
alfentanil, and propofol were described as a potential contributing
factors, however, pre-treatment with anti-cholinergic agents
may reduce this incidence in healthy individuals, and hence
bradycardia under anaesthesia shouldn’t be assumed as
iatrogenic as the cause might be sick sinus syndrome [6]. Bearing
the following in mind, it was deemed necessary to expedite the
patient to theatre and to commencing of CPB to avert further
injury to the heart and avoid peri-arrest episodes.
Yet and despite the measures undertaken to correct the
underlying ischaemic causes that potentially led to acute intraventricular stunning of the conduction system, the patient
persistently continued to display signs of tachyarrhythmia and
even after a PPM was sought for. This is a unique experience
that opens the scope for further studies or models to predict
occurrence of asymptomatic intraventricular conduction
abnormalities prior to CABG and to overall correctable causes.
A.H. has prepared the first draft of the case report. M.B.
has reviewed and made necessary changes in the case report.
M.L. has reviewed the final manuscript and made changes. N.R.
reviewed and approved final manuscript.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php
To know more about Juniper Publishers please
click on: https://juniperpublishers.business.site/



Comments
Post a Comment