Heart Failure in Afro-Caribbean: A Cardiovascular Enigma-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Introduction
Heart failure is a disease in which there are
striking population differences in almost every aspect of the disease.
It has been recognized that the cause of heart failure is predominantly
ischemic disease in nonblack but is related primarily to hypertension in
blacks and this statement should be also assessed in Afro-Caribbean
patients because population differences in disease exist that may be
attributable to differences in social factors, genetics, environment,
lifestyle, comorbidities, and complex interactions among these factors.
The full impact of cardiovascular disease risk
factors on incident disease and cardiovascular mortality in the
Caribbean community is still not known, as there are not longitudinal
studies on incident or fatal cardiovascular disease [1]. Data from St
James Study in Trinidad showed that Blood Pressure, diabetes and low
density lipoprotein were independent predictors of coronary heart
disease in men [2] while data from the Barbados Registry of Stroke
showed that of the patients with incident Stroke in Barbados, 68% had a
history of hypertension and 38% had Diabetes [3], however we lack of
local information on the incidence of heart failure (HF) in the
Afro-Caribbean community. There are several population based studies of
HF in Afro-Caribbean in the UK. A re-analysis of a hospital based audit
in Birmingham [4] indicates that the risk of HF for African Caribbean,
compared to Europeans, in those aged 60-79 years was 3.1 (95% confidence
limits 1.9 to 4.9). In adult African Americans the prevalence of HF has
been estimated at 3%-higher than white counterparts [5]. This is not
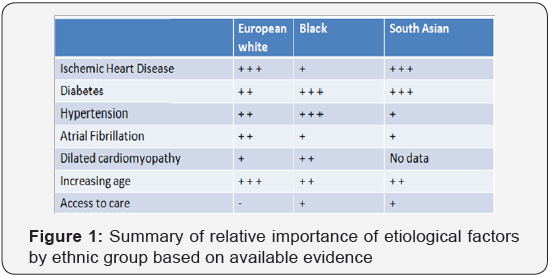
explained by coronary artery disease, as the prevalence of CAD (Figure
1) is lower in
black patients with HF [6]. Both the prevalence of the risk factor and
its associated risk for the outcome are needed to determine the
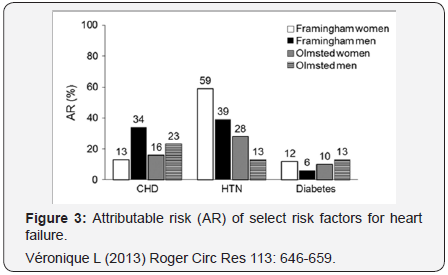
population impact of a risk factor on a disease. Coronary disease,
hypertension, diabetes, obesity, and smoking has been each associated
with an increased risk for HF (Figure 2 & 3), but the Population
Attributable Risk -PAR- has been shown to be greatest for coronary
disease (20%) and hypertension (20%) in the Olmsted County Study [7].
Again, data on the burden of HF in diverse populations are scarce.

In ARIC and in the Multi-Ethnic Study of Atherosclerosis
(MESA), HF incidence was higher in blacks than in whites. In
both studies, the difference between blacks and whites was
attenuated after adjustment and overall the greater HF incidence
in blacks was related to their greater burden of atherosclerotic
risk factors as well as to socioeconomic status [8,9]. Data on the
incidence and prevalence of HF according to EF and how it may
have changed over time are very limited. The available evidence
suggests that the prevalence of HF with preserved EF increased
over time [10]. Studies of Caribbean Heart Failure are scarce.
In the only study of Heart Failure (n=100), published ten years
ago in a private practice in Jamaica, GR Lalljie & SE Lalljie [11]
reported that most patients were over 65 years of age, female,
never smoked cigarettes, overweight/obese and hypertensive
(82%). The main etiologies were hypertension (54%) and
ischemic heart disease (IHD) (26%). Ninety-one per cent were
in sinus rhythm and 6% in atrial fibrillation.
Forty-nine per cent had echocardiograms, of these 39%
had ejection fractions (EF) >40%, 34% had EF 21-40% and
27% had EF <20%. Hypertensive heart disease was found in
54%, hypertensive cardiomyopathy in 14% and ischemic heart
disease in 26%. According to the most recent census, conducted
in 2011, the majority of Jamaicans identify as black [12] the
ethnic groups are [13]: Black (92.1%), Mixed (6.1%), Asian
(0.8%), other (0.4 %). Much of Jamaica’s black population is of
African or partially African descent with many being able to trace
their origins to West Africa. It has been previously observed that
Coronary Heart Disease (CHD) and Peripheral Arterial Disease
(PAD) are less prevalent among Afro-Caribbean compared to
Caucasian and South East Asian ethnic groups. The prevalence of
CHD range from 0-7% in Afro-Caribbean to 2-22% in Caucasians.
Strokes are more common among Afro-Caribbean,
unfortunately, there are inadequate data on morbidity and
mortality from cardiovascular disease (CVD), particularly across
the socio-economic gradient, in Afro-Caribbean populations
[14]. Previous study of the Jamaican prevalence of hypertension
estimated HTN in 30.8% in the 15-and-over age group [15];
however a more recent study has shown that the prevalence
estimates for traditional CVD risk factors are: hypertension,
25%; diabetes, 8%; hypercholesterolemia, 12%; obesity, 25%; smoking 15%. [1]. Therefore it is obvious that the burden of
cardiovascular disease risk factors in Jamaica And in comparison
in parallel with other communities of the Caribbean remains
very high. Evidence-based therapies for heart failure (HF)
differ significantly according to left ventricular ejection fraction
(LVEF). However, few data are available on the phenotype and
prognosis of patients with HF with midrange LVEF of 40% to
55% (HFmrEF), and the impact of recovered systolic function
on the clinical features, functional capacity, and outcomes of
this population is not known [16]. Previous investigations in
American [17] and Chinese [18] populations have demonstrated
that subjects with HF and a normal EF (>55%) -HFNEF, differ
in their clinical and demographic characteristics from subjects
with mildly (40% to 55%) and severely (<40%) decreased EF.
Differentiation of patients with HF based on LVEF is important
due to different underlying etiologies, demographics, comorbidities
and response to therapies [19] however there are
not comparative research among Afro-Caribbean patients with
HF with midrange EF (HFmrEF) vs HF with reduced EF (HFrEF).
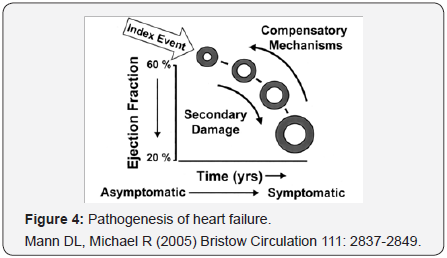
Heart failure (HF) is usually a progressive condition
(Figure 4) that begins with risk factors for LV dysfunction (e.g.,
hypertension), proceeds to asymptomatic changes in cardiac
structure (e.g., LV hypertrophy) and function (e.g., impaired
relaxation), and then evolves into clinically overt HF, disability
and death [20]. It is difficult to know in which proportion
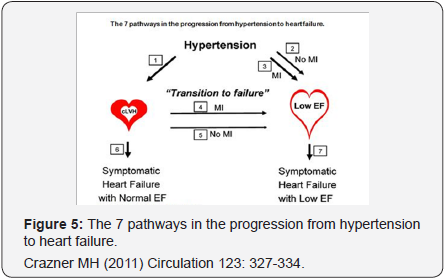
hypertensive patients evolved towards one of the different possibilities of Hypertensive heart disease (HHD). It is now
well recognized that clinical heart failure can occur either in the
setting of reduced LVEF or normal-preserved-LVEF. The potential
progression of asymptomatic LV dysfunction to clinical heart
failure in Hypertensive patients has been elegantly reviewed
by Drazner [21]. He has proposed seven possible pathways in
the progression from hypertension to heart failure (Figure 5):
Hypertension progresses to concentric (thick-walled) LVH
(cLVH; pathway 1). The direct pathway from hypertension to
Dilated Cardiac Failure-DCF (increased LV volume with reduced
LVEF) can occur without (pathway 2) or with (pathway 3) an
interval myocardial infarction (MI).
Concentric hypertrophy progresses to dilated cardiac
failure
(transition to failure) most commonly via an interval myocardial
infarction (pathway 4). Recent data suggest that it is not common
for concentric hypertrophy to progress to DCF without interval
myocardial infarction (pathway 5) and patients with concentric
LVH can develop symptomatic heart failure with a preserved
LVEF (pathway 6), or patients with DCF can develop symptomatic
heart failure with reduced LVEF (pathway 7). There are other
influences of other important modulators of the progression of
hypertensive heart disease, including obesity, diabetes mellitus,
age, environmental exposures, and genetic factors. Hypertensive
heart disease simulating dilated cardiomyopathy (DCM) has
been previously documented [22], these patients had past
history of hypertension and prominent left ventricular dilatation
with reduced left ventricular contractility, but no left ventricular
wall thickening. Among cases reported by Lalljie [11] 14% were
considered as Hypertensive cardiomyopathy. In what proportion
and for what reason, pathophysiological, biological or ethnic,
some Afro-Caribbean patients, almost all of them hypertensive
with or without diabetes, develop Dilated Cardiac Failure with
severe LVSD but with normal epicardial coronary arteries
(angiographically proven) and how many of them with the
same risk profile develop non-ischemic dilated cardiomyopathy
-NIDCM (angiographically proven) is a topic that we do not know
and that deserves to be considered and investigated. In short, the
consideration of a direct pathway from Hypertension to dilated
hypertensive heart disease (DHHD) seems to be plausible. From
another point of view, perhaps not all patients considered DHHD
hypertensive are really a form of Hypertensive heart disease. In
211 Afro-Caribbean patients with heart failure presenting to St
George’s Hospital Heart Failure clinic [23] the most common
cause of heart failure was nonischemic dilated cardiomyopathy
(NIDCM) in 27.5% (whites, 19.9%; P<0.001). Lower rates of
ischemic cardiomyopathy were observed (13% versus 41%;
P<0.001). Interesting, the fourth most common cause of heart
failure in Afro-Caribbean living in UK, was cardiac amyloidosis
(11.4%). Since Caribbean countries do not routinely perform
testing for cardiac amyloidosis (ATTR V122I), it is possible that
some of these subjects with DHHH or NIDCM may be confused
with other etiologies. According with Dungu et al. [24] about 4% of
African-Americans possess the V122I variant of transthyretin,
associated with cardiac amyloidosis (ATTR) and ten percent of
Afro-Caribbean heart failure population have ATTR V122I, often
misdiagnosed as hypertensive heart disease (HHD), however,
they founded that differential diagnosis of ATTR V122I over
HHD could be strongly supported when the ventricular septum
thickness exceeds precordial voltage [24].

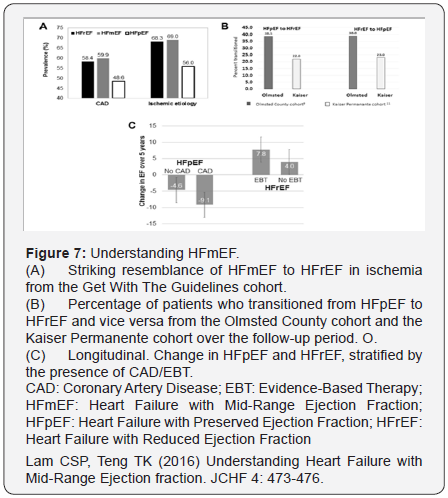
Patients with an LVEF in the range of 40-49% represent a
‘grey area’: The current HF Guidelines have mentioned that
identifying HFmrEF as a separate group can stimulate research
into the underlying characteristics, pathophysiology and treatment of this group of patients (Figures 6&7). Patients
with HFmrEF most probably have primarily mild systolic
dysfunction, but with features of diastolic dysfunction [25].
Aging has been associated with diastolic dysfunction. On the
other hand, in a cohort of Chinese patients [18] with mildly
decreased EF (40% to 55%), despite the only mildly dilated left
ventricular dimensions by 2-dimensional echocardiography,
they had significant ventricular remodeling (e.g., rightward
shift in end-diastolic pressure–volume relation) and decreases
in chamber contractility. The researchers comment that this is
markedly different from the physiologic parameters displayed
in the cohort with HF and EF >55%, and more similar to the
phenotype observed in patients with overt systolic HF (with an
EF <40%). Nadruz et al. [16] have concluded that patients with
HF with midrange LVEF demonstrate a distinct clinical profile
from HFpEF and HFrEF patients, with objective measures of
functional capacity similar to HFpEF. Within the midrange LVEF
HF population, recovered systolic function is a marker of more
favorable prognosis. With current understanding, HFmrEF is
distinct from HFrEF (EF < 40%) simply because there is no
evidence-based therapy, and distinct from HFpEF (EF ≥ 50%)
simply because EF is not preserved [26]. For now we do not
have information on this new category in the Afro-Caribbean
community.
Heart failure (HF) has been singled out as an epidemic and is
a staggering clinical and public health problem, associated with
significant mortality, morbidity, and healthcare expenditures,
particularly among those aged ≥65 years. The case mix of
HF is changing over time with a growing proportion of cases
presenting with preserved ejection fraction for which there
is no specific treatment. (30 In the E-ECHOES Study [27] of
Prevalence of Heart Failure and Atrial Fibrillation in Minority
Ethnic Subjects 17 Afro Caribbean -AC, (0.89%; 95% CI 0.52 to
1.42%) had an LVEF <40% with a mean age of 72.4 years (SD
11.0), of which 15 (88.24%) were males. The proportion of
patients with hypertension was 57.9% and diabetes 26.3%. Just
1.36% Afro-Caribbean patients of this cohort had evidence of
atrial fibrillation with a mean CHADS2 score of 2.3. Assigning
a cause to HF should be envisioned while focusing on clinically
ascertained risk factors and acknowledging that multiple causes
for HF often coexist and interact in a given patient [28]. It has
been established that the etiology of HF is diverse within and
among world regions. There is no agreed single classification
system for the causes of HF, with much overlap between
potential categories (Diseases Myocardium, Abnormal loading
conditions or Arrhythmias). Many patients will have several
different pathologies-cardiovascular and non-cardiovascularthat
conspire to cause HF. Indeed, the Identification of these
diverse pathologies should be part of the diagnostic workup, as
they may offer specific therapeutic opportunities. Many patientswith HF and ischemic heart disease (IHD) have a history of
myocardial infarction or revascularization. However, a normal
coronary angiogram does not exclude myocardial scar (e.g.
by CMR imaging) or impaired coronary microcirculation as
alternative evidence for IHD [25].
The prevalence and incidence of left bundle branch block
in Afro-Caribbean patients with HFrEF is not well known and
must be assessed as it could underlines the importance of
Myocardium Diseases in the Afro-Caribbean population . It has
been widely studied that LBBB may occur in asymptomatic
individuals, patients with extensive myocardial infarction, and
in those with heart failure, especially in dilated, non-ischemic
cardiomyopathies. In some patients, LBBB (sometimes rate
dependent) may be the first manifestation of heart disease
whereas the clinical presentation of a dilated cardiomyopathy
develops only some years later [29]. The fact that a proportion
of Afro-Caribbean patients with HFrEF have wide QRS complex
(LBBB), should stimulate to consider more resources directed
to Cardiac Resynchronization Therapy (CRT) in the Caribbean
community as CRT has been recommended for symptomatic
patients with HF in sinus rhythm with a QRS duration ≥150msec
and LBBB QRS morphology and with LVEF ≤35% despite OMT,
in order to improve symptoms and reduce the HF morbidity and
mortality [25].

According with Sanderson [30], HFrEF is mainly due to
myocardial infarction or dilated cardiomyopathy that rapidly
damages the myocardium, whereas in HFNEF (HFpEF), the
effects of hypertension (HTN), diabetes, and aging are slower
and would explain why some measurement of LV mechanics
(i.e. long-axis function, which is a more sensitive measure) can
be reduced while EF remains “normal”. He emphasizes that
cardiologists working in Africa, East Asia, and India often can
see patients with HFrEF who have only HTN as a risk factor, and
presumably these patients passed through an HFpEF (HFNEF) phase, however other risk factors may interact, including alcohol
intake, which has experimentally-induced HFrEF with a typical
dilated LV with low EF in spontaneously hypertensive rats with
pre-existing LV hypertrophy and a normal or supranormal
EF). Accordingly, the Time course and pattern of development
of heart failure (Figure 8) is primarily caused by myocardial
infarction (MI), with pronounced remodeling and shape change
leading to systolic heart failure (SHF), and HF primarily caused
by hypertension (HT), with or without diabetes mellitus (DM),
leading to heart failure with , initially, a normal ejection fraction
(HFNEF). Patients with a history of MI and patients with HTN
may experience periods of HFNEF and finally they develop
systolic heart failure with a reduced ejection fraction (HFrEF).
Assuming that the Afro American Heart Failure data could be
applied to the Afro-Caribbean community it appears that HF in
this region to be of worse severity that HF in white patients. The
clinical experience suggests that at the time of diagnosis, left
ventricular function seems to be more severely impaired and
the clinical class is more advanced. There is no doubt that the
strongest risk factor for heart failure in Afro-Caribbean seems
to be hypertension, which is both more prevalent and more
pathologic in Afro-Caribbean population. It is likely that heart
failure represents an important end organ effect of hypertension.
When affected by heart failure, Afro-Caribbean might experience
a greater rate of hospitalization and may be exposed to a higher
mortality risk as well. Genomic medicine has yielded a number
of candidate single nucleotide polymorphisms that might
contribute to the excess pathogenicity of heart failure in African
Americans [31], but much more work needs to be done in larger
cohorts. Effective therapy of heart failure must start with the
recognition of the different manifestations of heart failure in
African Caribbean.
An increased awareness of the risk of hypertension followed
by early and effective intervention may reduce the risk of heart
failure in this population. The SOLVD Registry [32] was the
first trial to demonstrate a significant difference in the putative
etiology of LV dysfunction in African Americans with heart
failure. It is reasonable to assume that documented ischemic
heart disease as a cause of heart failure occurs less frequently
in the African Caribbean patient than other groups of patients,
an observation that was also initially put forward by analysis of
the SOLVD Registry. In summary, Afro-Caribbean hypertensive
patients would evolve for an initial phase with normal EF (HFNEF
or HFpEF) and depending on the associated pathophysiological
and risk factors or the severity of hypertensive cardiovascular
disease they eventually develop systolic dysfunction, initially
mild (HFmrEF) and finally severe ( HFrEF). The impact of an
effective therapy (OMT) on reverse remodeling may further
change this complex final outcome.
After The Vasodilator–Heart Failure Trials I and II, there
remain many promises and unanswered questions regarding
Hydralazine-Isorbide Dinitrate (H-ISDN) therapy in heart failure, ranging from efficacy and mechanism of action to
defining optimal patient population and timing of therapy [33].
It had already been confirmed (Figure 9) a lesser response
to angiotensin-converting enzyme inhibitors (ACEIs) and
β-blockers in lowering blood pressure in black versus nonblack
hypertensives [34], but (Figure 10) The African-American Heart
Failure Trial (A-HeFT) found that the addition of a fixed-dose
combination of isosorbide dinitrate/hydralazine to standard
neurohormonal blockade resulted in a 43% improvement in
survival, a 33% reduction in hospitalizations for heart failure,
and significant improvement in quality of life measured with the
Minnesota Living With Heart Failure questionnaire [35]. These
striking improvements in outcomes occurred in patients welltreated
with standard neurohormonal blockade, including ACE
inhibition, angiotensin receptor blockade, and β-blockade. This
outcome suggested that alternative or additional mechanisms
of progression of heart failure, perhaps related to impaired
nitric oxide availability, were present in this population and
were treated by this combination. Considering the persistent
suboptimal outcomes and a significant opportunity for
improvement in therapy for these patients, further research
related to the use of H-ISDN in heart failure in Afro-Caribbean
population seems warranted.


In summary, Heart failure is a disease in which there are
striking population differences in almost every aspect of the
disease. It has been recognized that the cause of heart failure
is predominantly ischemic disease in nonblack but is related
primarily to hypertension in blacks [36] and this statement
should be also confirmed in Afro-Caribbean patients because
population differences in disease exist that may be attributable
to differences in social factors, genetics, environment, lifestyle,
co-morbidities, and complex interactions among these factors.
The term African Caribbean needs to be defined and restricted
to an African descent person originating from the Caribbean.
The concept of ethnicity encapsulates cultural, behavioral, and
environmental factors that increase the risk of disease; hence it is
crucial in epidemiology and public health [37]. When population
differences are observed, focused studies are warranted to
identify the contribution of these factors (including biological,
environmental, social, genetic, and lifestyle factors and their
interactions) and how best to treat them. Identification and study
of population differences may enhance disease treatment in all
populations and additionally may provide disparity-reducing
benefit for populations with poorer health outcomes [38-40].
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php
To know more about Juniper Publishers please
click on: https://juniperpublishers.business.site/



Comments
Post a Comment