Dose Response Study of Intrathecal Morphine for Off-Pump Coronary Artery Bypass Grafting: a pilot Prospective Randomized Double-Blinded Controlled Clinical Trial-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Objective: To determine the optimal
dose of intrathecal morphine in patients undergoing off-pump coronary
artery bypass grafting (OPCAB) surgery.
Design: A prospective, randomized, double-blinded, placebo-controlled study.
Setting:
A tertiary-level university teaching hospital.
Participants: 31 adult patients scheduled for elective primary OPCAB surgery.
Interventions: Patients were
randomized to receive 2.5μg/kg (ITM-2.5) or 5μg/kg (ITM-5) intrathecal
morphine or sham-control preoperatively. Anaesthesia was induced and
maintained with sufentanil (limited to 1μg/kg), propofol, rocuronium and
isoflurane. Blinded observer-caregivers extubated the patients using
protocol-defined criteria, and on-demand intravenous morphine (IVM) was
administered to patients using a standardized protocol.
Measurements and Results: Blinded
observers measured the time to extubation, the amount of supplemental
IVM used in the first 48hours post-extubation, satisfaction with pain
control, ICU discharge time, hospital discharge time, the incidence of
vomiting, pruritus, urinary retention. Pain at rest (VASR) and during
movement (VASM) were scored using the Visual Analogue Scale at 2, 4, 8,
24, 36 and 48 hours from extubation. ITM 2.5μg/kg was as effective as
5μg/kg, and superior to on demand IVM alone. VAS values in ITM-2.5 and
ITM-5 groups were similar, and significantly lower in first 24hours
comparing to the control group at rest as well as during coughing
(p<0.05). The 48hour cumulative dose of IVM was 22±12mg, 28±14mg, and
36±18mg in ITM-5, ITM-2.5, and control groups respectively. Fewer cases
of pruritus, PONV and urinary retention were reported in the ITM-2.5
compared with the ITM-5 group. There were no differences among the study
groups with regard to extubation time, ICU discharge and hospital
discharge time.
Conclusion: ITM of 2.5μg/kg was
superior to IVM analgesia regimen. Furthermore, it had similar
effectiveness and fewer side effects compared to ITM of 5μg/kg. This
study suggests that the optimal effective dose of ITM is 2.5μg/kg for
OPCAB surgery for postoperative analgesia.
Abbrevations:ITM: Intrathecal Morphine; IVM: Intravenous Morphine; OPCAB: Off-Pump Coronary Arterial Bypass; VASR: Visual Analogue Scale at Rest; VASM: Visual Analogue Scale on Movement
Introduction
Patients undergoing off-pump coronary artery bypass
grafting (OPCAB) surgery are suitable for Ultra-Fast-Track protocol
including tracheal extubation in the operating room
[1,2]. This approach has been associated with a restriction of
intraoperative opioid administration, in order to preserve the
respiratory drive upon awakening after surgery and may lead to
inadequate postoperative analgesia. Intrathecal Morphine (ITM)
provides effective postoperative analgesia in major surgery [3,4]
with a low risk of epidural haematoma [5,6]. Recent studies have
shown that ITM provides effective postoperative analgesia in
cardiac surgery [7,8]. But what is unclear from the literature is
the minimal effective dose of ITM for cardiac surgery, especially
in the context of OPCAB surgery, whose patients are suited to a
fast-track extubation protocol.
Our goal was to determine the optimal dose, whilst
minimizing the side effects of ITM in patients undergoing
OPCAB surgery. We hypothesize that 2.5μg/kg of ITM would not
be inferior to 5μg/kg of ITM with respect to adequacy of pain
control and side-effect profile.
After receiving permission from the UHN Research Ethics
Board, we recruited 31 patients scheduled for OPCAB surgery
and obtained their written consent to participate in this
prospective randomized double-blinded controlled clinical trial.
Patients were excluded from the study if they had
contraindications to regional anaesthesia such as local sepsis,
anticoagulation, non-elective surgery, left ventricular ejection
fraction (LVEF) less than 40% or if they refused consent.
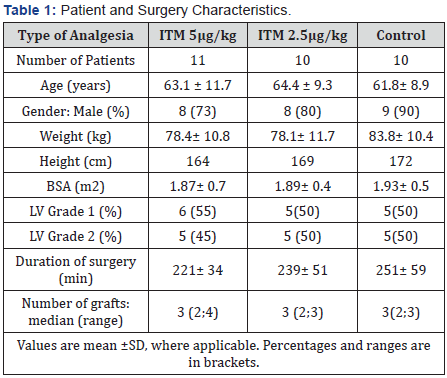
A total of 31 patients were studied (Table 1). Of the 31
patients, 11 were randomized to the (ITM-5) 5μg/kg intrathecal
morphine group, 10 to the (ITM-2.5) 2.5μg/kg and 10 to the
sham-control groups respectively. A computer-generated
randomization was used in the allocation to the groups. All
patients, intraoperative caregivers and ICU caregivers were
unaware of the group allocations. All groups had comparable
demographic data, co-morbidities and surgical characteristics
(Table 1).
The preparation of intrathecal morphine was provided
by
pharmacy staff to ensure blinding. The administrations of ITM
were performed by an anesthesiologist not directly designated
to the patient’s perioperative care. Patients were either placed in the
sitting or lateral decubitus positions. The skin was prepared
with chlorhexidine, and 2-5mL of 2% lidocaine local anesthetic
was injected subcutaneously at L2-3 or L3-4 levels by palpation.
A midline approach was used for ITM administration. The
designated dose of intrathecal morphine (5 or 2.5μg/kg) madeup
to volumes of 3mL, this was then administered via a 25 G
Whitacre spinal needle via introducer into the intrathecal space.
All patients were given local anesthetic subcutaneously, only the
sham-control group did not receive an intrathecal puncture. The
puncture site was covered by adhesive dressing.
General anesthesia was established with intravenous
sufentanil at 0.5 to 1μg/kg, propofol and rocuronium as deemed
appropriate by the designated anesthesiologist, and general
anesthesia was maintained with isoflurane in oxygen and air
mixture. Isoflurane was stopped at time or just prior to skin
closure. Propofol infusion was started at 50μg/kg/min after
skin closure for the transfer to the ICU. There was no restriction
on the use of intravenous fluids, blood products, vasopressors,
inotropes, vasodilators or anti-arrhythmics in order to maintain
haemodynamic stability at the discretion of the designated
anesthesiologist.
Sedation was maintained with propofol infusion titrated to
a Ramsay sedation score of 3 to 4. The criteria used for tracheal
extubation included:
- Patient responsive and cooperative.
- Negative inspiratory pressures <-20cm H2O.
- Vital capacity >10mL.kg-1.
- Arterial oxygen tension (PaO2) >80mm Hg and FiO2 ≤0.5, v) cardiac index >2.0 L.min-1.m2.
- Core temperature >36.5°C.
- pH >7.30.
- Chest drain output <100mL/h for 2 or more hours.
The ICU nurses performed extubation, and “on-demand”
IV morphine (IVM) analgesia according to the standardized
protocol [9]. Postoperative pain was treated with morphine,
0.5 to 5mg intravenously, as required. Shivering was controlled
by 25 to 50mg of intravenous meperidine. Persistent systemic
hypertension (systolic blood pressure >140mm Hg) was treated
with infusion of nitroglycerin and/or nitroprusside, adjusted
to a systolic arterial pressure between 90 and 130mm Hg.
Intravenous boluses of 10-20mg esmolol were used to control
persistent tachycardia >110 BPM.
All measurements were performed by an observer who was
blinded to the patient’s designated group. The analysis of the
outcome variables using the intention-to-treat principle. Visual-
Analogue-Scale was used to assess analgesia at rest (VASR),
and during “on-demand” movement by coughing (VASM) at 2,
4, 8, 24, 36 and 48 hours from end of extubation. All patients
were asked to indicate their pain score on the VAS from the 2
hour mark onwards. At each juncture, pain scores were firstly recorded at rest, and immediately followed by a score at cough
on-demand. Total supplemental intravenous morphine used
and the incidence of morphine related side-effects of vomiting,
pruritus and urinary retention within the first 48 hours were
recorded. At a day 5 questionnaire, each patient was asked
whether they were “satisfied” or “not satisfied” with the
analgesia they received.
ICU discharge criteria included:
- Patient alert and cooperative.
- No inotropic support and no significant arrhythmia.
- Adequate ventilation (PaO2 >80mm Hg, PaCO2 < 60mm Hg.
- Chest drain output < 50mL/h for 2 or more hours.
- Urine output >0.5mL.kg-1.h-1.
- Absence of seizure activity.
The time of ICU discharge was the time of the written order
for transfer out of the ICU, as documented by the blinded fellow
or anaesthesiologist in-charge. The actual physical discharge
time of the patient from the ICU was also recorded. Hospital
discharge criteria included:
- Haemodynamic stability.
- Stability of cardiac rhythm.
- Absence of wound infection or signs of sepsis.
- Adequate urination and defaecation.
- Independent ambulation and feeding.
Time of hospital discharge was likewise recorded as per the
time of written documentation of discharge order by the blinded
ward physician in-charge.
The sample size was limited to a pilot study. Categorical
and numerical data were analyzed with Fisher’s exact test
and analysis of variance respectively. A p value of 0.05 was
considered statistically significant. Bonferroni correction was
applied for multiple testing. Data are expressed as mean ±SD or
median (range).
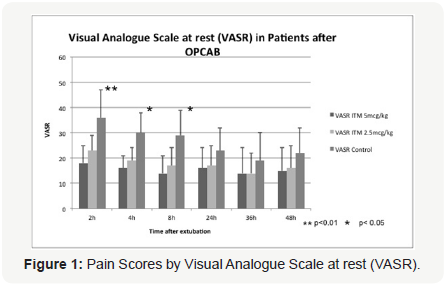
Pain scores at rest by VAS (Figure 1) were significantly lower
in the ITM-2.5 and ITM-5 groups when compared with control
at 2, 4 and 8 hours after extubation. There was a non-significant
decreasing trend in pain scores at 24, 36 and 48 hours. The ITM-
2.5 and ITM-5 groups did not differ significantly in pain scores at
rest at all time intervals. P-value was significant at the 0.01 level
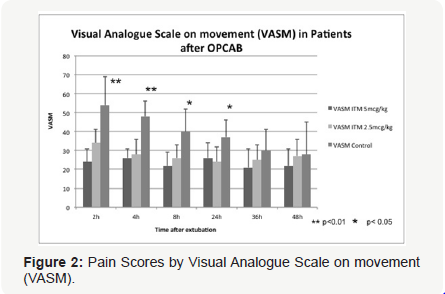
at 2 hours, and at the 0.05 levels at 4 and 8 hours. Similarly, pain
scores on movement by VAS (Figure 2) were significantly lower
in the ITM-2.5 and ITM-5 groups when compared with control at
2, 4, 8 and 24 hours. P values were significant at the 0.01 level at
2 and 4 hours and at the 0.05 level at 8 and 24 hours. There was
a non-significant decreasing trend in pain scores at 36 and 48
hours. Once again the ITM-2.5 and ITM-5 groups did not differ in
pain scores on movement at all time intervals.
The 48h cumulative dose of IVM was 22 ±12mg, 28 ±14mg,
and 36 ±18mg in ITM-5, ITM-2.5 and control groups respectively
(Table 2). However, the decreasing trend in morphine use from
ITM-5 to ITM-2.5 to control group did not reach statistical
significance.
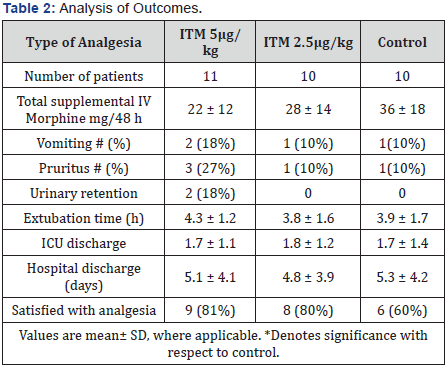
With regard to adverse side-effects, 2 of the 11 patients in
the ITM-5 group experienced urinary retention compared with
0 of 10 patients respectively in the ITM-2.5 and control groups. 2 patients in the ITM-5 groups suffered from PONV compared with
1 patient in the ITM-2.5 and 1 patient in the control group. 3 of
the ITM-5 patients complained of pruritus compared with 1 in
the ITM-2.5 and 1 in the control group. There was no difference
in the extubation time, ICU discharge time, hospital discharge
time for the 3 groups in this study.
There were no instances of traumatic tap or spinal
haematoma in this study. Activated clotting time were kept at
<400 seconds by heparin. There were no conversions to onpump
CABG./p>
Intrathecal morphine has been shown to be effective in
postoperative analgesia in both cardiac and non-cardiac major
surgery. A study comparing two doses of ITM in on-pump CABG
surgery suggests 250μg is preferred to 500μg ITM, without
delaying tracheal extubation [8]. In a meta-analysis by Liu
et al. [10] which included 17 RCTs and a total of 668 patients
undergoing, they found that the use of intrathecal morphine
in patients undergoing CABG surgery decreased times to
extubation, pain scores and IV morphine use postoperatively
[10].
However, the optimal dosage of ITM is not known for
effective postoperative analgesia, especially in the context of
OPCAB surgery. In the previously mentioned meta-analysis10,
which varied in opioids used in induction, maintenance and
postoperatively, ranges of dosing varied between 250μg and
2000μg; weight-adjusted dosing varied [11,12] between 7μg.
kg-1 to 20μg.kg-1. Given such a wide range of practice in the
literature, RCTs such as our present study are called for in
the determination of a minimal effective dose of ITM in CABG
surgery.
In this study of OPCAB patients, ITM of 2.5μg/kg was
superior to on-demand IVM analgesia regimen for postoperative
analgesia and not inferior to ITM of 5μg/kg. VAS values in ITM-
2.5 and ITM-5 groups were similar, and significantly (p<0.05)
lower in first 24 hours compared to the control group at rest as
well as during coughing on-demand (Figures 1 & 2). However
after the 24 hour mark, there was loss of statistical significance
despite a continued trend toward lower VASR and VASM in the
ITM-2.5 and ITM-5 groups compared to the control group. None
of the patients had any apneic episodes related to ITM with
the 48 hour observation period. In a similar RCT in patients
undergoing OPCAB surgery comparing no ITM with 10μg/kg
ITM led by Turker et al. [13] patients significantly scored less
on VASM even at the 24 and 48 hour mark [13]. It appears that if
ITM were at a significantly higher level of 10μg/kg or more, then
we expect longer postoperative analgesic effect. The question
becomes how to balance optimal postoperative analgesia that
provides good conditions for early extubation and patient
satisfaction, whilst minimizing the side-effects of ITM.
Crucial to the study findings was blinding of the investigators,
the designated case-anesthetist, the operator placing the
intrathecal morphine, the patients, the care giver and the
observer in ICU. The obvious point of weakness in blinding is
the experience of the patient who did not receive intrathecal
morphine: he or she would have been given subcutaneous
local anaesthetic alone, without the second puncture that
necessarily accompanies the delivery of intrathecal morphine.
But the subjection of patients to placebo intrathecal puncture
was deemed to be an unethical intervention. Hence blinding
was considered as best as possible amongst the patient groups,
without causing unnecessary harm to the placebo group. Patients
would have to have had prior intrathecal puncture experience
and recalled the experience exactly, in order to differentiate
themselves from the placebo group and the ITM-2.5 or ITM-
5 groups. From the postoperative questionnaire, there was no
suggestion that patient blinding had failed.
In a similar vein, there was a decreasing trend in the
cumulative 48 hour intravenous morphine use from control to
ITM-2.5 to ITM-5 groups. This was a secondary outcome and
surrogate marker of the efficacy of postoperative analgesia of
ITM and the trend is in keeping with both older and recent studies
of postoperative analgesic efficacy of intrathecal morphine
in cardiac surgery [7,14,15] although Chaney [16,17] and
Roedinger et al. [18] have revisited their previous conclusions
[16-18] on the significance of ITM in post-operative analgesia.
Despite not being the primary aim of this study, the findings are
in agreement with the general consensus that ITM does provide
significant postoperative analgesia in cardiac surgery and is
superior to intravenous morphine on-demand alone.
Furthermore the ITM-2.5 group, compared to ITM-5, had
lower incidences of PONV and urinary retention, which are wellknown
side effects of opioid analgesics. There was a trend toward
shorter extubation time in the ITM-2.5 and control group when
compared with the ITM-5 group, but this was not statistically
significant. The present study findings are in keeping with other
studies on ITM in cardiac surgery [9,19] in that ITM did not
seem delay extubation; some have gone as far as to say the use
of ITM may improve extubation times because of improved pain
control in the postoperative period [20]. There is still an ongoing
dialogue on whether early extubation is favored or impaired
by ITM preoperatively [21]. The sample was underpowered to
show the statistical difference between incidence of PONV and
pruritus between the ITM-2.5 and ITM-5 groups.
We support the use of 2.5μg/kg intrathecal morphine
preoperatively as an optimal dose in patients undergoing CABG
surgery, especially those suitable for fast-track extubation, such
as those undergoing off-pump CABG surgeries. This study was
not adequately powered to make definite conclusions regarding
major morbidity and mortality. We recommend larger clinical trials on the minimal effective dosing of intrathecal morphine in
both off-pump and on-pump CABG surgery, to support and verify
the finding of this study.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment