Surgery is Still Alive in Descending Thoracic Aortic Aneurysm-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY &
CARDIOVASCULAR THERAPY
Abstract
Introduction: The surgical treatment
of descending thoracic aortic aneurysm is changing in response to the
advent of endovascular treatment; however, not all of patients are
candidates for it. The choice of the surgical technique isessential at
the moment of taking these patients to conventional surgery.
Case Report: A 25-year-old female
patient with a symptomatic descending thoracic aortic aneurysm of 54 x
53 mm after coarctation surgery of the aorta in childhood who was
operated in a conventional manner through complete circulatory arrest.
She was discharged at 5 postoperative days without central or peripheral
neurological complications.
Conclusion: Aneurysm after aortic
coarctation surgery is a late complication known. The most serious
complications of conventional repair of these have been neurological,
both central and peripheral. With the technique proposed by Dr. Chard,
we demonstrate once again that surgery can be performed with low
morbidity and mortality.
Introduction
Surgical treatment for descending thoracic aneurysm
is changing drastically in response to the advent of endovascular
treatment. The endoprosthesis has been used to treat DTA with favorable
results.
However, replacement by conventional surgery is still
the standard treatment for DTA. There are several surgical strategies
for DTA such as single clamping, distal perfusion by left heart bypass,
hypothermic circulatory arrest and partial cardiopulmonary bypass [1].
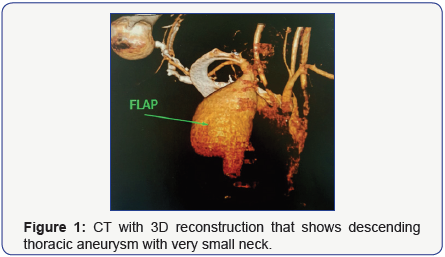
A 25-year-old female patient with a history of
coarctation of the aorta operated at the age of 6 presents with a
symptomatic descending thoracic aortic aneurysm (chest pain) of 54 x 53
mm in diameter and 75.4 mm in length by MRI, which involves the
Subclavian artery (Figure 1). Due to the diameter of the proximal neck
of 17.5 mm and impossibility of endovascular treatment in our center,
conventional surgical treatment was decided.
The patient was anesthetized with an endotracheal
double lumen tube, positioned in the right lateral position, keeping the
torso at 45º and the legs at 90º. The thoracotomy was performed at the
level of the 4ª intercostal space. Left common femoral venous
cannulation was performed guided to the right atriumby TEE and then
femoral arterial cannulation on the same side.
A thorough dissection of the left lung with large adhesions was
performed until the DTA was reached and then CPB was started,
during which the patient cooled until reaching 17ºC, after which
the heart was stopped without arrhythmia. Circulatory arrest
was started. The aneurysm was sectioned longitudinally. The
left subclavian artery was identified as the reason for which a
descending aorta was replaced with Dacron prosthesis of 18
mm. After that, the subclavian artery was reinserted by the
interposition of 8 mm Dacron prosthesis.
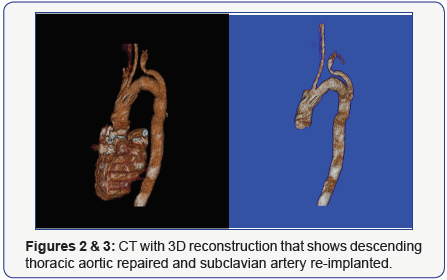
Subsequently raffia of the aneurysmal sac was performed on
the implanted prosthesis. After all the anastomosis, the patients
were gradually re-heated and the onset of CPB started again.
Surgery without aortic clamping was performed by means of
a circulatory arrest of 52 minutes and total time of ECC of 150
minutes. The patient was extubated within the first 8 hours after
surgery in the intensive care unit, without central or peripheral
neurological complication. Normal postoperative course and she
was discharged after 5 days. Currently, he performs activities
according to his age and the correct repair of his initial aneurysm
was verified by CT scan with contrast at 90 days postoperatively
(Figures 2 & 3).
Despite the advances in brain protection and surgical
techniques, brain damage remains a frequent complication,
particularly as a cerebral infarction after aortic clamping.
Different techniques such as selective cerebral perfusion,
hypothermic circulatory arrest and retrograde cerebral
perfusion associated with hypothermic circulatory arrest have been used in aortic arch operations [2].
The formation of aneurysm at the site of a previous coarctation
repair is increasingly recognized as a late complication and is
more frequently associated with the use of prosthesis repair. The
incidence varies between 5 and 38% occurring between 6 and
18 years after aortoplasty [3].
Surgical intervention of post-coarctation aortic aneurysms
involves difficulties related to clamping of the aorta such as
cerebral infarction, bleeding, dissection, medullary ischemia and
recurrent laryngeal nerve injury, including surgical adhesions
that increase the technical difficulties [4].
In our case, we decided to perform the technique proposed
by Dr. Chard because of the high risk of injury of the recurrent
laryngeal nerve by completely sectioning the aorta and the need
of replantation of subclavian artery.
According to the technical difficulties that this type of
surgery presents, not only the need of reoperation but also
the high risk of spinal cord injury and peripheral nerves, we
recommend by means of the presentation of our case, the
realization of circulatory arrest and deep hypothermia, as well
as longitudinal section of the aneurysm without total resection
to avoid those complication, in patients who are not good
candidates for TEVAR. Conventional surgery can be performed
with low morbidity and mortality if the appropriate technique is
used in the appropriate patient.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment