Clinical Outcomes after Intravascular Ultrasound Assessment of Coronary Intermediate Lesions-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Purpose: Coronary angiography
has limitations in the assessment of intermediate coronary lesions
(ICL). Intravascular ultrasound (IVUS) can evaluate more accurately the
severity of a lesion to guide the therapeutic strategy. This study
sought to evaluate long-term clinical outcomes after IVUS-guided
coronary revascularization of ICL lesions in patients from the Western
Mediterranean region of coastal North Africa (Maghreb) in whom IVUS
severity criteria have not been validated.
Methods: We conducted a
prospective monocentric study including 113 patients with angiographic
ICL evaluated by IVUS. Minimal lumen area (MLA) cut-offs value to
perform revascularization were 6 mm² for the left main coronary artery
(LMCA) and 4 mm² for non- LMCA lesions. The primary outcome was defined
as a composite of major adverse cardiac events (MACE) including death,
myocardial infarction (MI), and target lesion revascularization (TLR) at
12 months.
Results: Mean age was 59,5 ±
12,0 years, 79% were men. Multi-vessel disease was present in 65.5% of
our patients, of whom 36 patients had LMCA disease. We analysed 146
arteries with 178 lesions. Revascularization was deferred for n=46
(40.7%) patients after IVUS evaluation. After a mean follow-up of 20± 10
months, we observed no significant differences between the
revascularized patients and the patients with a deferred
revascularization strategy in terms of mortality (1.5% and 2.2%
respectively, p=0.7), and a favourable safety trend for 12-month rate of
MACE (10.6% and 2.2% respectively, p=0.165), MI (4.5% and 2.2%, p=0.44)
and TLR (10.7% and 2.2%, p=0.23).
Conclusion: We demonstrate that
previously validated IVUS criteria to defer revascularization of
angiographically ICL can be safely applied to Maghrebi patients.
Abbreviations: ICL: Intermediate Coronary Lesions; IVUS: Intra Vascular Ultra Sound; FFR: Fractional Flow Reserve; MACE: Major Adverse Cardiac Events; MI: Myocardial Infarction; TLR: Target Lesion Revascularization; LMCA: Left Main Coronary Artery; LAD: Left Anterior Descending Artery; MLA: Minimal Lumen Area; PB: Plaque Burden; LL: Lesion Length; RD: Reference Diameter; PCI: Percutaneous Coronary Intervention; CABG: Coronary Artery Bypass Graft; NSTEMI: Non ST Elevation Myocardial Infarction; STEMI: ST Elevation Myocardial Infarction
Introduction
Clinical decision making and the management of
intermediate coronary lesions (ICL) continues to be a therapeutic
dilemma for cardiologists. The limitations of coronary angiography for
the evaluation of such lesions are well recognized since 20 years [1],
and adjunctive diagnostic techniques have been developed. Intravascular
ultrasound (IVUS) offers the possibility to base decisions not only on
lumeno grams but also on true lumen and vessel size and plaque
accumulation in the coronary wall. The IVUS criteria reported in the
literature defining a functional significant coronary stenosis have been
recently reassessed and compared with the fractional flow reserve (FFR)
derived from intracoronary pressure measurements. The princeps criteria
of a significant stenosis based on a lumen area less than 4 mm² has
been challenged by numerous investigators proposing down to
2.1 mm² [2-16].
However, many of these studies were only reporting a head
to head comparison with a FFR cut off of 0.75 or 0.8 without
outcome data, while a recent prospective study of nearly 700
patients demonstrated that ICL with a lumen area <4 mm² were
associated with three more times major adverse cardiovascular
events [17]. The aim of this study was to evaluate long-term
clinical outcomes in patients from Western Mediterranean
region of coastal North Africa (Maghreb) where IVUS studies
so far have not been conducted and reported. In these patients,
Percutaneous coronary intervention of angiographically ICL was
decided on the basis of the IVUS findings using criteria reported
in Western population and Asia but so far not prospectively
assess in this region of North Africa characterized by a high
incidence of diabetes mellitus and hypertension [18,19].
Study population: Between October 2010 and December
2013, we conducted a prospective monocentric study including
113 patients with angiographically ICL who underwent IVUS
assessment to decide whether to perform or not revascularization.
Patients with acute myocardial infarction, significant distal
lesions, those in whom the IVUS-imaging catheter failed to cross
the lesion due to severe stenosis or tortuosity and small vessels
(reference diameter <2.5mm) were excluded. The primary
outcome was defined as a composite of major adverse cardiac
events (MACE) including death, myocardial infarction (MI), and
target lesion revascularization (TLR) at 12 months.
Angiographic analysis: Coronary angiography was
performed with GE Innova® 2000 and Innova® 2100 IQ
interventional cardiology systems. Visual estimation of lesion
severity, length and reference diameter was performed and
reported on the CARDIOREPORTTM database by a single
operator who proposed an initial therapeutic strategy. All
lesions were classified according to the ACC/AHA consensus
[20]. All ICL, defined by a diameter stenosis of 30% to 50% for
the left main coronary artery (LMCA) and 40% to 70% for non-
LMCA lesions, were revaluated on a heart team staff, and IVUS
evaluation was decided each time that there was no unanimity
on the therapeutic strategy.
IVUS analysis: Intravascular ultrasound guidance was
performed using conventional 6-F guiding catheters and a 0.014-
mm guide wire positioned distally, and 40 MHz IVUS catheters
(Boston Scientific®) pulled back automatically at a constant
speed of 0.5 mm/s. After imaging acquisition the lumen-intima
and media-adventitia interfaces were measured at the target site
following the guidelines of the American College of Cardiology
[21]:
- Minimal lumen area (MLA);
- plaque burden (PB);
- lesion length (LL); and
- Reference diameter (RD).
MLA cut-offs value to perform revascularization were 6 mm²
for the LMCA and 4 mm² for non-LMCA lesions.
Clinical Data, Definitions, and Outcomes: Hospital records
of all patients were reviewed to obtain information on clinical
demographics and medical history. Follow-up information
was obtained through review of hospital charts or telephone
interviews. The primary outcome was defined as a composite
of major adverse cardiac events (MACE), including death,
myocardial infarction (MI), and target lesion revascularization
(TLR) at 12 months. Death was defined as cardiac mortality.
The diagnosis of myocardial infarction was based on either the
development of new pathological Q waves in ≥ 2 contiguous
electrocardiogram leads and/or cardiac enzyme level elevation
3 times the upper limit of normal value. TLR included target
lesion percutaneous coronary intervention (PCI) and bypass
surgery of the target lesion (CABG).
Statistical analysis: Statistical analysis was performed
using IBM® SPSS® Statistics version 20 for Windows. Data
are expressed as mean ± SD for continuous variables and as
percentages for discrete variables. The normal distribution
of variables was verified by the Kolmogorov-Smirnov test for
normality. Categorical data were compared using chi-square
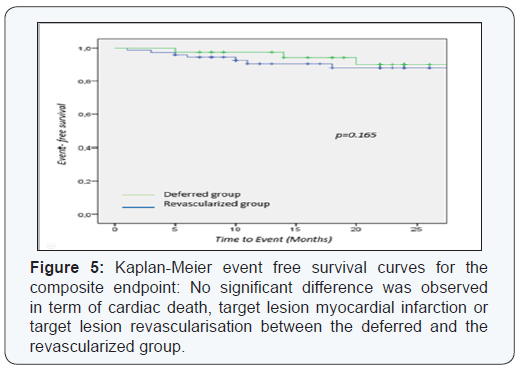
test. Event-free survival curves were established using the
Kaplan-Meier estimation. All calculated p values were 2-sided
and differences were considered to be statistically significant
when the respective p values were < 0.05.

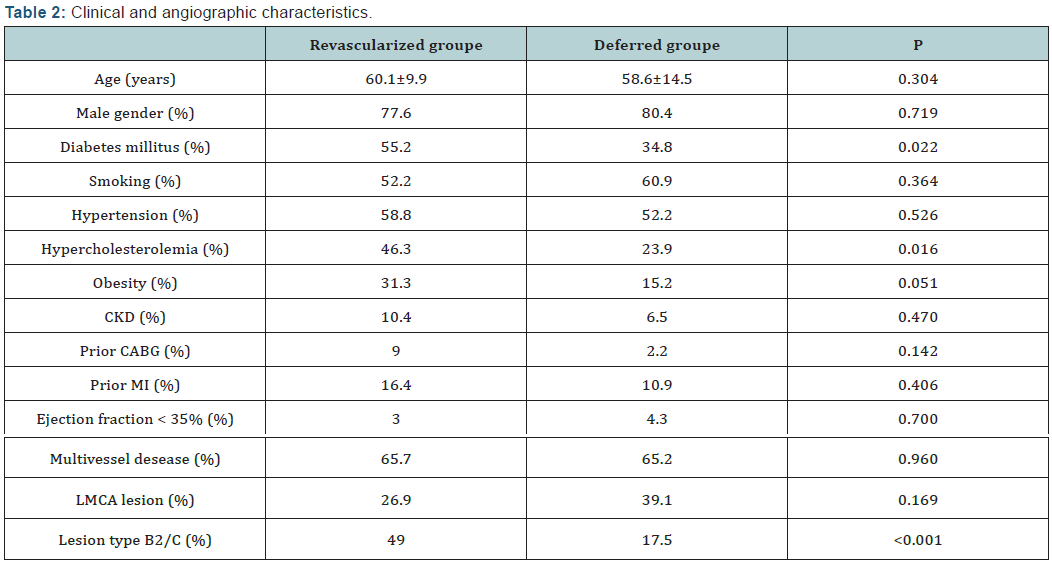
A total of 113 consecutive patients were included, 146
arteries and 178 lesions were analysed. Baseline clinical
characteristics, angiographic and IVUS finding are summarized
in (Table 1). Complete follow-up data were available for 112
patients over a mean follow-up time of 20 ± 10 months. There
was no protocol violation and all patients with MLA values below the defined cutoffs underwent either PCI or CABG. Overall
revascularization was deferred for 46 patients (40.7%) after
IVUS assessment. There were significantly more patients with
diabetes mellitus, hypercholesterolemia and complex lesions in
the revascularized group (Table 2).
The majority of parents (92%, n=225) and children (54%,
n=133) were female. The average age of child was six years
ranging from one to nine years? The presence of siblings was
identified by 32 respondents (12%). In terms of ethnicity, a
majority of the parents identified their children as White (53%,
n=131) followed by Black (21%, n=52) and multiple/mixed
(20%, n=49), Asian (5%, n=11) and other (1%, n=3) ethnic
groups. Here in after, respondents will be referred to as parents.
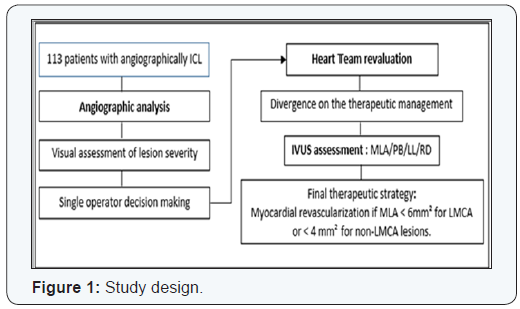
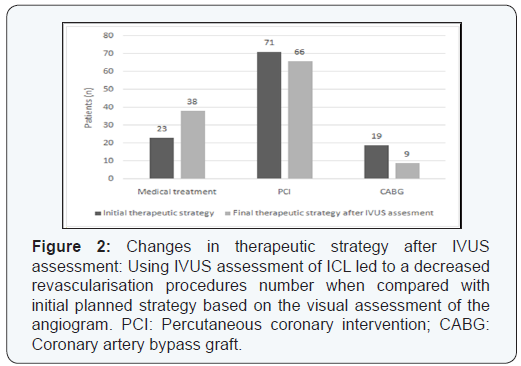
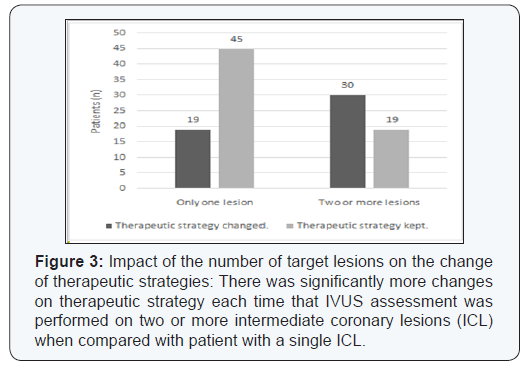
Decision making:
31% of the LMCA lesions and 41% of the non-LMCA
lesions that were angiographycally estimated more than
50% stenosis were not significant as assessed by IVUS (p<0.01). This
discordance resulted in a change in the therapeutic strategy in
49 patients (43.3%) with a significant reduction in the indications of
revascularization: 81.6% of the initial PCI or CABG indications
in this group were delayed. This was significantly more frequent
with lesions involving the LMCA and the proximal left anterior
descending artery or when there were 2 or more intermediate
lesions to evaluate (Figures 1-4).

Major adverse cardiovascular event at 12 months followup:
Overall, 12 patients presented a major cardiac event after a
mean follow-up of 20 ± 10 months. In the deferred group, only
one cardiac death was reported and one patient presented a MI
for which he underwent PCI. There were two cardiac deaths.
One patient died after complications of bypass surgery and the
second from a NSTEMI complicated by cardiogenic shock, after
proximal LAD PCI was not performed in basis of IVUS finding.
Three MI occurred: two patients had NSTEMI related to late
stent thrombosis, and one patient had anterior STEMI one month
after he underwent IVUS assessment for an ICL in the proximal
LAD (MLA = 8.61 mm²). During the 12-month follow up period,
10 TLR were performed. Nine patients had PCI; eight with DES
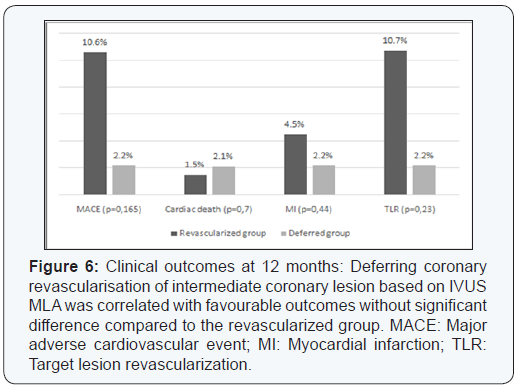
and one with BMS. Only one patient had CABG. We observed no significant differences between the revascularized patients and
the patients whose revascularization was postponed in terms
of mortality (1.5% and 2.2% respectively, p=0.7), 12-month
rate of MACE (10.6% and 2.2%, p=0.165), myocardial infarction
(4.5% and 2.2%, p=0.44) and 12-month rate of target lesion
revascularization (10.7% and 2.2%, p=0.23) (Figures 5 & 6).
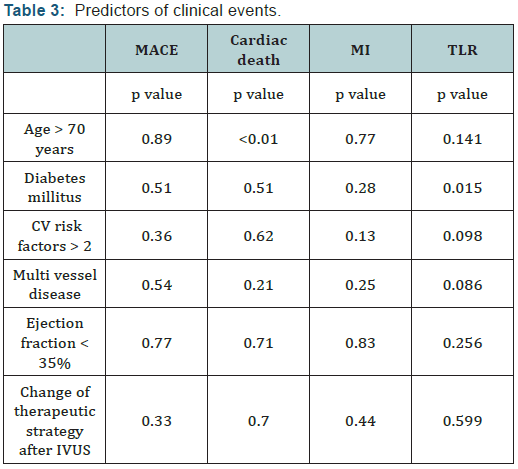
No cardiac events occurred during the first 12 months follow
up for all the patients with LMCA ICL in whom revascularization
was deferred. Age and diabetes mellitus were the only significant
univariate predictors of, respectively, cardiac death (p<0.01) and
TLR (p=0.015). The change of the therapeutic strategy after IVUS
evaluation was not correlated with significant change in events
rates (Table 3).
The present study showed the following:
- There was a poor correlation between visual angiographic estimation and IVUS MLA assessment of a coronary stenosis severity,
- This led to a change of therapeutic strategy in 43.3% of cases,
- The use of a MLA cut-off value of 4 mm² for the non-LMCA stenosis and 6 mm² for the LMCA stenosis, was correlated with favourable outcomes.
The limitations of coronary angiography in assessing
lCL severity have been well documented. The inter-observer
variability is high and little further information is gleaned
from computer-assisted quantitative angiography [1,22-24].
IVUS has been used since the 1990’s to assess the severity of
intermediate coronary stenosis and several studies proved
the good correlation between MLA and the physiological
significance of such lesions. Its incremental diagnostic value
was proven repeatedly for the most challenging lesions, those
of the left main (LM). Sano et al. [25] reported three times more
significant lesions by IVUS among 115 consecutive patients with
a de novo, angiographically ambiguous, intermediate LM lesions,
compared to QCA [25].
The cut-off value for lumen area to predict ischemia is still
disputed, and range from 2.1 to 4.4 mm² [2-16,26] for the non-
LMCA lesions and 4.8 to 7.5 mm² [27-30] for the LMCA lesions. In
53 non LMCA intermediate lesions, Briguori et al [16] reported
that an MLA cut off of 4 mm² was the best IVUS parameter
correlated with identifying FFR < 0.75 with 92% sensitivity
and 56% specificity. However, recent studies have found lower
MLA cut off values and have used a combination of other
IVUS parameters to predict FFR. In a multicenter, prospective,
international registry of 350 patients with 367 intermediate
coronary lesions (FIRST: Fractional Flow Reserve and
Intravascular Ultrasound Relationship Study) [12], Walksman et
al. reported that an MLA < 3,07 mm² (64.0% sensitivity, 64.9%
specificity, area under curve [AUC] = 0.65) was the best threshold
value for identifying FFR <0.8. Same results were founded
by Ben Dor et al. [8] with improved accuracy when reference
vessel-specific analyses were performed. Trials conducted in
East Asia population have reported even lower MLA cut off, Kang
et al. [26] established that the best cut off value of the MLA to
predict FFR <0.80 was <2.4 mm², with a diagnostic accuracy of
68% (90% sensitivity, 60% specificity).
Few studies compared IVUS finding with FFR as the “gold
standard” for determining the functional significance of LMCA
ICL. In an analysis of 55 western patients, Jasti et al. [27] reported
that an MLA < 6 mm2 strongly predicted FFR < 0.8 (sensitivity
and specificity of 93% and 95%, respectively). Lower MLA cutoff
was again reported in Asian population; Kang et al. suggested
that 4,8 mm² was the best MLA cutoff correlated to an FFR < 0,8
with 89% sensitivity and 83% specificity.
Care must be taken in the interpretation of these studies
conducted in different populations, many in Japan and Korea
where there is a large usage of IVUS in the cat lab. There is
presently no IVUS report from North Africa / Arabic countries characterized by a higher incidence of smoking, diabetes
mellitus, and hypertension.
Different studies had reported that using IVUS to guide
decision making induced a significant change in the therapeutic
strategy. Mintz et al. [31] reported that pre intervention
IVUS imaging performed in 301 patients led to a change on
revascularisation therapy in 121 patients (40%). A higher rate of
change in clinical decision after IVUS assessment was reported
by other authors (60 to 70,6%) [32-34]. However there is few
clinical trials that established the clinical safety of using IVUS
MLA to defer a myocardial revascularization. The chosen MLA
cut-off thresholds to defer revascularization in those studies
were 4mm² for the non-LMCA ICL [35-37] and 6mm² [28,38]or
7.5 mm² [29] for the LMCA ICL (Table 4).
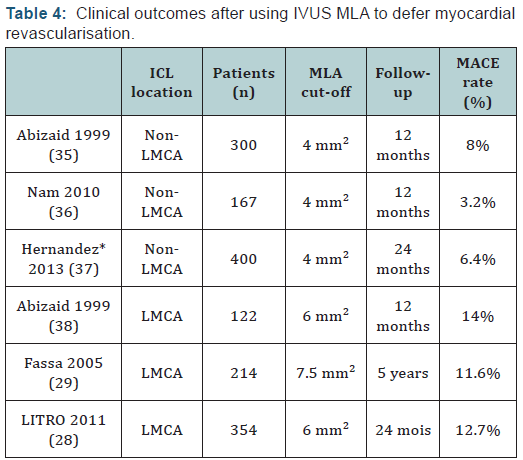
In 300 patients with non LMCA ICL, deferring PCI on the
basis of an IVUS MLA ≥ 4.0 mm2 was associated with a low
rate of events (8% at 12 months) [35]. Clinical safety of this
MLA cut off was confirmed by others studies showing even
fewer cardiac events [36,37]. Otherwise, compare to FFR based
decision making, Hernandez et al. [37] reported that even if IVUS
assessment led to more revascularization procedures, there was
no significant differences in MACE-free survival (97.7% at one
year and 93.1% at two years in the FFR group and 97.7% at one
year and 95.6% at two years in the IVUS group; p=0.35) and
among those with deferred intervention (97.9% at one year and
94.2% at two years in the FFR group and 96.5% at one year and
93.6% at two years in the IVUS group; p=0.7).
For the LMCA ICL, different studies reported that using the
IVUS MLA to defer myocardial revascularisation is also correlated
with favourable outcomes [28,29,38]. In the LITRO study [28],
which enrolled 354 patients with LMCA ICL, there was no
significant difference between the deferred and revascularized
groups in terms of cardiac death-free survival (97.7% vs 94.5%,
respectively, P = 0.5) and event-free survival (87.3% vs 80.6%, respectively, P = 0.3) after a mean follow up of 24 months. Our
study confirmed the high negative predictive value of this MLA
cut-off and accordingly the clinical safety of delaying myocardial
revascularization of ICL based on IVUS evaluation.
Study limitations: Principal’s limitations of the present study
are:
- The limited number of included patients due to economic difficulties in an emergent region where IVUS prone are not reimbursed by any insurance funds. We estimate that only one in four patients with ICL underwent IVUS analysis.
- The MLA cut off value of 4 mm² chose to perform revascularisation on non-LMCA lesions might to appear too high (and well above the ischemic threshold) [12], and
- The lack of clear criteria to make the initial therapeutic decision which was at the operator’s discretion.
The use of IVUS in a population from Maghreb to assess
angiographically intermediate coronary lesions is correlated
with a significant decrease of myocardial revascularization
indications and favourable long term outcomes.
Conflict of Interest: The authors declare that they have no
conflict of interest.
Ethical approval: All procedures performed involving
human participants were in accordance with the ethical
standards of the national research committee. There were no
animal study.
Informed consent: Informed consent was obtained from all
individual participants included in this study.
For more articles in Open Access Journal of Cardiology & Cardiovascular
Therapy please
click on:
https://juniperpublishers.com/jocct/index.php
https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment