Sequential Observation of Angio-SealTM-Induced Acute Limb Ischemia vie Angiography and Intravascular ultrasound-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Femoral artery stenosis and occlusions are relatively common following the use of Angio-SealTM
devices compared with other vascular closure devices (VCDs). This study
reports the first such case that we could observe the absorption of the
collagen plug one year after balloon angioplasty for Angio-SealTM-
induced acute limb ischemia in the angiographic and IVUS finding. A
66-year-old male with effort-induced angina pectoris underwent
percutaneous coronary intervention (PCI) for severe stenosis of the
proximal left anterior descending artery (LAD) through a right femoral
artery access. A 7 Fr, 11 cm sheath was inserted through the right
femoral artery. The puncture site was closed with an 8 Fr Angio-SealTM
device after the completion of the PCI. Patient’s right popliteal
artery and dorsalis pedis artery became impalpable about one hour after
the procedure.
Emergency angiography revealed subtotal occlusion
(99%) of the proximal right superficial femoral artery (SFA). Emergency
endovascular treatment of the right SFA was performed through a left
femoral artery access. Balloon dilatation was performed with a 5.0 ×
40-mm balloon resulting in improvement of antegrade flow. Severe
stenosis persisted (area stenosis rate was 85%) immediately after EVT.
Follow-up IVUS and angiography one year after procedure demonstrated
gradual absorption of the collagen plug, with a reduction in vessel
stenosis and symptomatic improvement. These findings suggest that
balloon dilatation and close monitoring constitute an effective strategy
for the management of Angio-SealTM-induced acute limb ischemia.
Abbreviations:IVUS: Intravascular Ultrasound; EVT: Endovascular Therapy ; SFA: Superficial Femoral Artery; VCDs: Vascular Closure Devices; LAD: Left Anterior Descending Artery; PCI: Percutaneous Coronary Intervention; ABI: Ankle-Brachial Index
Introduction
Vascular closure devices (VCDs) are commonly used
following trans-femoral interventions to achieve immediate hemostasis.
Femoral artery stenosis and occlusions are relatively common following
the use of Angio- SealTM devices (St. Jude Medical, Austin,
Texas). However, acute limb ischemia accompanying such instances is a
rare but serious complication. Conventionally, this complication is
managed by surgical revascularization or endovascular therapy (EVT). It
is a problem for EVT that the component of the Angio-SealTM remains in the
blood vessel. Some reports that the intravascular component of the Angio-SealTM is absorbed almost completely within 90 days of deployment. The absorption of component of the Angio-SealTM
to vessels in human has not been previously reported. This study
reports the first such case that we could observe the absorption of the
collagen plug one year after balloon dilatation therapy for Angio-SealTM-induced
acute limb ischemia in the angiographic and intravascular ultrasound
(IVUS) finding. The absorption of the collagen plug one year after
endovascular therapy resulted in the reduction in the stenosis, as well
as symptomatic improvement.
was admitted to our hospital for effort-induced chest pain.
Coronary angiography revealed severe stenosis in the proximal
left anterior descending artery (LAD), and percutaneous
coronary intervention (PCI) for an LAD lesion was performed
after accessing the right femoral artery. The Ankle-brachial
index (ABI) on the right side was 1.1 and on the left side was
1.15. Femoral artery diameter was 7.4 mm on the right side and
there was no evidence of any stenosis. Prior to the procedure,
he received aspirin (100 mg/day) and clopidogrel (75 mg/day)
for seven days. A 7 Fr, 11 cm sheath was inserted into the right
femoral artery. Sheath insertion was immediately followed by an
intravenous injection of 5000 units of heparin. A drug-eluting
stent (24 x 3.5mm) was deployed in the proximal LAD, and the
puncture site was closed with an 8 Fr Angio-SealTM device.
The patient complained of pain in the right calf and a
feeling of coldness in the tips of his toes, one hour following
the procedure. Examination revealed impalpable right popliteal
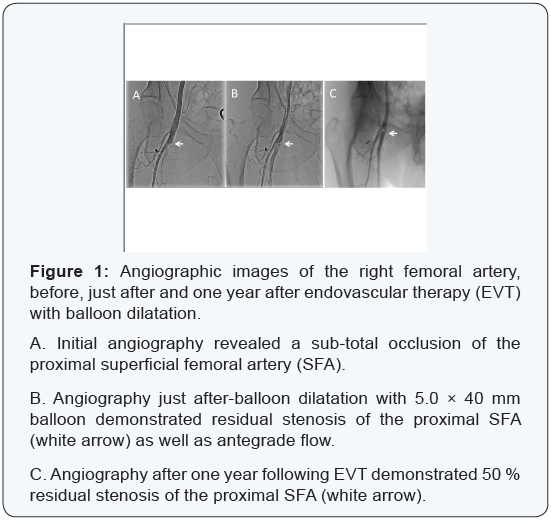
and dorsalis pedis artery. Emergency angiography, performed
through the left femoral artery revealed subtotal occlusion
(99%) of the proximal right superficial femoral artery (SFA)
(Figure 1). Emergency endovascular therapy (EVT) of the right
SFA was performed through a left femoral artery access. A 0.014
guidewire (CruiseTM, Asahi Intecc Co. Ltd., Aichi, Japan) was
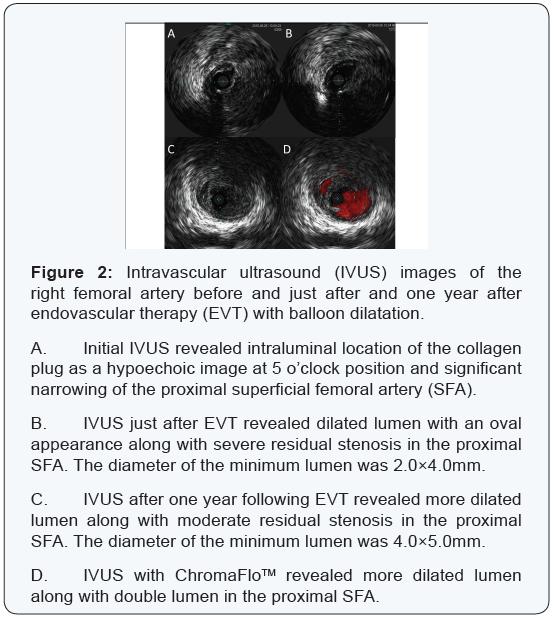
passed across the lesion. Intravascular ultrasound (IVUS; Vision
PVTM 018, Volcano Co. Ltd., San Diego, CA, USA) demonstrated the
collagen plug of the Angio-SealTM present intraluminally (Figure
2). Balloon dilatation was performed with a 5.0 × 40 mm balloon
catheter with a long inflation time of up to 2 minutes. Postdilatation
IVUS demonstrated that the SFA diameter was 2.0 ×
5.0 mm, which appeared to be insufficient for perfusion (Figure
2), and severe stenosis of the right proximal SFA persisteed.
However, since there was an improvement in the antegrade flow,
the procedure was terminated (Figure 1b). The patient reported
relief of calf pain, and increased warmth in the periphery of his
right foot immediately following the procedure. However, he
complained of intermittent claudication. B-mode sonography
performed five days after EVT identified the intraluminal
collagen plug as a hypoechoic lesion and measured the diameter
percent stenosis as 85%.
Following EVT, the patient was started on anticoagulant
treatment with apixaban (20 mg/day), in addition to double
antiplatelet therapy with aspirin and clopidogrel. Apixaban was
stopped two months after EVT, while aspirin (100 mg/day) and
clopidogrel (75 mg/day) were continued. Four months after the
procedure, he no longer complained of intermittent claudication.
His ABI on the right side improved from 0.47 just after EVT
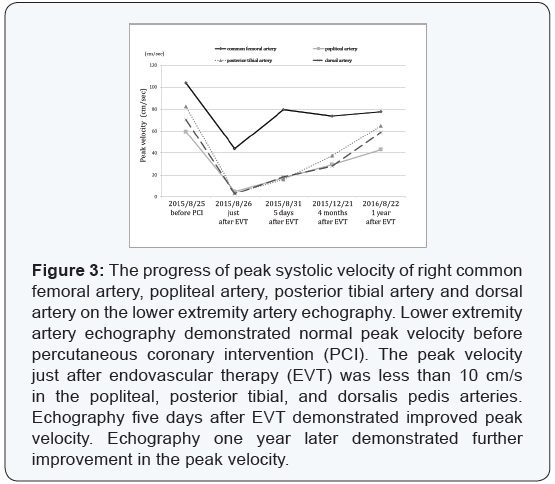
to 0.98 at about one year following the procedure. On lower
extremity artery echography, the peak velocity improved in the
popliteal artery (from 17.5 cm/s [5 days following EVT] to 43.0
cm/s [about 1 year following EVT]), posterior tibial artery (from
16.2 cm/s to 65.0 cm/s), and in the dorsalis pedis artery (18.5
cm/s to 59.1 cm/s) (Figure 3). Angiography demonstrated 50 %
residual stenosis of the proximal SFA about one year after EVT
(Figure 1). Follow up IVUS about one year after EVT revealed
more dilated lumen along with moderate residual stenosis
in the proximal SFA and the diameter of the minimum lumen
was 4.0×5.0mm (Figure 2). Follow up IVUS with ChromaFloTM
revealed more dilated lumen along with double lumen in the
proximal SFA one year after EVT (Figure 2).
Hemorrhage, pseudoaneurysm, infection and vessel occlusion
are uncommon complications following the use of Angio-SealTM
devices. Although femoral artery stenosis or occlusion following
VCDs is rare, with the incidence of such complications ranging
from 0 to 2.9% [1], they are relatively common with the Angio-
SealTM device compared with other devices (Vaso-SealTM, St Jude
Medical Co. Ltd., St. Paul, MN, USA or TechstarTM, Abbot Vascular
Japan Co. Ltd., Calif, USA) [2]. Since acute limb ischemia or
leg necrosis may follow Angio-SealTM device-induced femoral
artery stenosis or occlusion, this is a serious complication. In
the present case, a technical difficulty was encountered during
deployment of the Angio-Seal device. The collagen plug could not
be easily inserted subcutaneously in spite of applying pressure
with the tamper tube. Therefore, it was forcibly positioned with
the aid of an inserter (PCI accessory device).
HThe collagen plug may have been forced into the vessel
lumen during these unplanned maneuvers, resulting in
superficial femoral artery (SFA) occlusion and thus, acute
limb ischemia. This was confirmed by both, the IVUS and the
lower extremity artery echography, which demonstrated the
intraluminal location of the collagen plug. The SFA diameter of 6
mm was adequate for the deployment of the Angio-SealTM device
[3]. However, this complication could be largely attributed to the
low position of the SFA puncture and the forcible insertion of
the collagen plug. The intravascular anchor of the Angio-SealTM is
expected to be absorbed with complete dissolution in about 30
days as observed on microscopy, and in 90 days as observed on
chemical analysis [4]. Tellez et al reports that the intravascular
component of the Angio-SealTM is absorbed almost completely
within 42 days of deployment as observed on IVUS [5]. In the
present case, about half of the anchor and collagen plug were absorbed over one year, resulting in a reduction in the stenosis,
as well as symptomatic improvement. The patient continued to
have residual stenosis and it was difficult to predict a further
reduction in the size of the collagen plug. In cases like this,
however, it is important to continue close monitoring of the
patient in anticipation of SFA restenosis or distal embolism.
There are some reports describing surgical revascularization
for Angio-SealTM -induced femoral artery stenosis or occlusion [6].
Surgical treatment must be considered for occlusions involving
large thrombus. In addition, stenting should be considered in
cases where balloon dilatation fails to open up the occlusion. In
the case of our patient, balloon dilatation alone provided relief
of acute limb ischemia. First, balloon dilatation achieved good
antegrade flow even in the absence of complete revascularization
of the SFA. Second, conservative therapy was followed by the
absorption of the collagen plug of the Angio-SealTM device as
confirmed by B-mode ultrasonography performed four months
following EVT. Balloon dilatation and close monitoring are less
invasive compared to surgical treatment; thus, this combination
is a useful strategy in the management of Angio-SealTM-induced
acute limb ischemia. It is important to consider the additional
reasons that could have contributed to the favorable response
of our patient to balloon dilatation alone. First, early detection
of acute limb ischemia resulted in emergency EVT without
much delay. Second, sub-total occlusion of the SFA instead of
complete occlusion may have enabled better antegrade blood
flow following EVT. Third, the patient received anticoagulation
with apixaban in addition to double antiplatelet therapy to avoid
thrombus formation.
For more articles in Open Access Journal of Cardiology & Cardiovascular
Therapy please
click on:
https://juniperpublishers.com/jocct/index.php
https://juniperpublishers.com/jocct/index.php


Comments
Post a Comment