Late-Onset Warfarin-Induced Skin Necrosis: A Standing Shadow-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
One of the clinical situations linked to the use
of warfarin is the skin necrosisoccurring in approximately 0.01 to 0.1%
of all patients receiving warfarin. Typically, lesions develop during
the first days after initiation of warfarin therapy (usually around the
tenth day) and are often associated with the administration of a loading
dose. The pathophysiological mechanisms for warfarin-induced skin
necrosis, despite several theories, remain uncertain. For the diagnosis,
along with a high degree of suspicion, a rapid recognition and
management is required.
Warfarin-induced skin necrosis (WISN) is a
complication of therapy with coumarinassociated with a high morbidity
and mortality [1]. In 1943, the necrotic changes were first time
described on the skinof a patient taking warfarin, at that time it was
called “disseminated thrombophlebitis migrans” [2] and were not related
to the use of warfarin. Later in 1954,Verhagen reported 13 confirmed
cases of warfarin-induced skin necrosis [3]. Overall, these lesions
occur in approximately 0.01 to 0.1% of all patients receiving warfarin
with a predilection for females in up to 90% of cases, beingthe typical
patient a middle-aged, obese, female withhistory of deep vein thrombosis
or pulmonary thromboembolism, with in most cases a reported protein C,
S, Factor V Leiden, and antithrombin III deficiency [4].
82 year old female palestinian patient with a medical
background of diabetes mellitus type II, essential hypertension and
ischemic dilated cardiomyopathy (New York Heart Association
Classification grade II), severe coronary three vessels disease
undergoing stenting in coronary descending artery nine years ago and
being a pacemaker holder due to a sick sinus node six months ago. In
addition she was diagnosed a chronic atrial fibrillation two years ago
being on warfarin since then, apart from other drugs to control her
multiple comorbidities. After a period of clinical stability for the
last three months, the patient was admitted in our hospital with a
diagnosis of acute pulmonary edemabeing treated in Intensive Care Unit
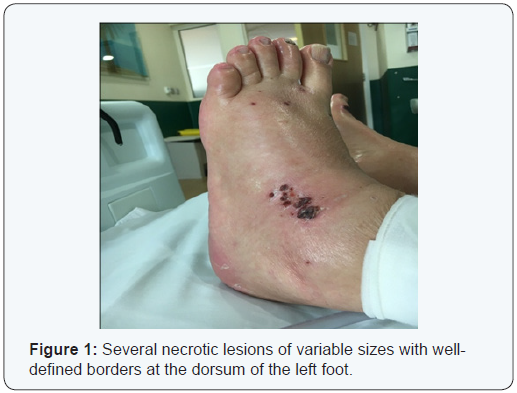
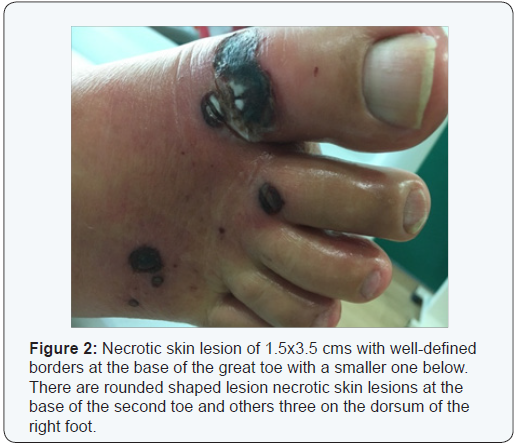
(ICU) with standard therapy. Moreover, upon first physical examination
in ICU were noticed some blisters with red borders filled with what
appeared to be a dark bloody contents on the skin of the dorsum of the
right foot and left footin number of three in each food with a variable
diameter, being the largest of 3 cm of diameter on the right foot and
tenderness upon palpation. After two days, there was a perceptible
improvement in the cardiac status of the patient and was transferred to
medical ward with still mild to moderate edemas in both feet. The
international normalized ratio (INR) was 1.8. The chest x ray showed
mild pulmonary congestion. The electrocardiogram revealed an atrial
fibrillation with normal ventricular response and by transthoracic
echocardiogram the ejection fraction was 35-40 %.
On day fourth of hospitalization, the lesions on both
feet looked like the ones shown in figure 1 and 2 being requested a
consultation with a dermatologist and a vascular surgeon whom after
their assessment stated that the patient was having a WISN. Immediately,
warfarin was discontinued and the patient was started of enoxaparin.
The lesion began to being treated topically with clobetazol in cream. At
that time was requested a blood protein C and S activity that came up
normal days after. After 10 days of thorough observation of the
progression of the lesions, there was an improvement of them indicating
signs of going into remission and with not need of further debridement.
Due to the improvement of the largestlesions after the warfarin’s
withdrawal and the disappearance of those in formation was
agreed not to perform a cutaneous biopsy. Subsequently, upon
discharge, enoxaparin was shifted to dabigatran for home
treatment.
The WISN as a complication of warfarin usage is uncommon.
Typically, lesions develop during the first days after initiation
of warfarin therapy (usually around the tenth day) and are
often associated with the administration of a loading dose.
The pathophysiological mechanisms for warfarin-induced skin
necrosis, despite several theories, remain uncertain, although,it
has been informed to be related with microvascular thrombosis,
hypersensitivity to warfarin and a direct toxic effect of the drug.
However, the most likely mechanism seems to be a temporary
imbalance between the anticoagulant-procoagulant system,
more specifically associated with a rapid decrease in C and S
protein levels during initial therapy with warfarin [5]. Regarding
the lesions associated with this condition, the patient first presents an erythematous rash poorly demarcated and often
associated with tissue soft edemaand paresthesias, subsequently
might appear petechiae progressing within hours to ecchymoses
and large hemorrhagic blisters that turn into afrank necrosis.
In most cases is a single lesion, although, up to one third of
cases can develop multiple lesions. These lesions can develop
at any part of the body, but have a predilection for high fat
areas like breasts, buttocks, thighs, arms, hands, fingers, legs,
feet, face and abdomen. In men, the lesions can affect the skin
of the penis [6]. For the diagnosis, along with a high degree of
suspicion, arapid recognition and management is required. Once
the lesions are recognized, stop warfarin must be the first step in
the treatment, and replace it by unfractionated or low molecular
weight heparin to prevent further thrombi formation. The use
of vitamin K and frozen fresh plasma for a quick replacement of
protein levels C and S is also suggested in these cases, in addition,
the treatment with protein C concentrates is postulated to stop
the progression of lesionsand promotes healing. It is also said
that over 50% of patients might require extensive debridement
and surgical management [7].
The late onset of WISN is very uncommon, few case have
been reported in the literature. However, there are reports of late
lesions onset up to three years after the initiation of warfarin
therapy. It is suspected that late-onset Warfarin-induced
necrosis is a result of poor compliance with Warfarin dosage
schedules, with the patient stopping and subsequently restarting
the medication without heparin coverage [8]. In our patient the
suspension of warfarin and its replacement with dabigatran,
stopped the progression of the lesions which were treated also
with a local steroid cream being noticeable the healing process
over time which took over one month. I would like to stress that
this case might represent another stepping stone to help break
the “old habit” of starting patients on warfarin for long term
anticoagulation-required disease and ponder the possibility of
drugs as dabigatran which has proved to be less harmful in terms
of side effects or use-related complications, besides a faster
onset and offset action, absence of an effect of dietary vitamin K
intake on their activity, and fewer drug interactions [9].
It is not about belittling the old and long live-saving warfarin,
it is about to know who will benefit or harm most when it comes
to begin anticoagulation treatment with warfarin. It is not
infrequent the initiation of treatment with warfarin in patients
who can afford new drugs as dabigatran, but the first choice in
our mind most time is warfarin and no doubts, in some patient
on the long run, warfarin will not do well and the skin necrosis is
like a shadow that always stands and might appear at any time.
For more articles in Open Access Journal of Cardiology & Cardiovascular
Therapy please
click on:
https://juniperpublishers.com/jocct/index.php
https://juniperpublishers.com/jocct/index.php


Comments
Post a Comment