Behavioral Cardiovascular Risk Factors: Changing Perspective to Approach the Problem-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Several studies indicate that psychological
factors strongly influence the neuro hormonal and behavioral
cardiovascular risk factors and the course of coronary artery disease
and event onset. New epidemiologic evidence for the association between
psychosocial risk factors and coronary artery disease identifies
pathologic mechanisms that may be responsible for this association. Not
much attention is paid to finding and managing the stressing factors
that provoke psychological distress and then multiple adverse peripheral
effects. This short review highlights a new way to look at the
behavioral risk factors; putting attention to what there is behind the
onset of stress and psychological distress that are related with
cardiovascular risk factors, atherosclerosis and events. The role of
cardiologist in finding out, assessing and managing stressors and
behavioral risk factors is emphasized and an emerging cardiological
field based on the understanding that psycho behavioral risk factors
require a new approach and a new more effective health care system is
suggested.
Keywords: Atherosclerosis; Behavioral risk factors; Neuro hormonal and Psycho behavioral structures; Stress
Atherosclerosis is a multi factorial disease of
polygenic inheritance and the interrelation with environmental and
social factors adds to complexity of the disease; in addition behavioral
risk factors contribute to atherosclerosis occurrence and development.
The relationship between risk factors and cardiovascular and
cerebrovascular diseases has been widely elucidated, including their
definition in unmodifiable (such as age, sex, familiarity, inheritance),
modifiable/curable (such as obesity, hypertension, physical inactivity,
dyslipidemia, diabetes) and psychosocial (such as stress, depression,
anxiety, type A personality, hostility and anger) [1-7]. The use of
traditional factors for risk stratification is well established and
those patients identified are at an increased risk. The long-term
follow-up of the Framingham Offspring cohort [8] allowed the
investigators to derive 30-year risk equations for hard and overall
cardiovascular event. However, depending on this traditional risk
factors, to assess individual risk might be late and, moreover, there
are difficulties to control it.
The European action on secondary prevention through
intervention to reduce events (EUROASPIRE) survey carried out in eight
European countries [9] reports that despite improvements in lipid
control, no significant changes in blood pressure levels or smoking were
obtained and increases in obesity and diabetes were seen in patients
with established coronary heart disease. On the other hand, traditional
risk factors for the development of atherosclerotic disease, which
accelerate the process over time and increase the risk of having a heart
attack, stroke or other arterial vascular problem are not present in 50
% of those who develop atherosclerotic problems [10]. These individuals
appear to have other genetic disorders or abnormal blood clotting,
chronic inflammation of arteries or as yet unknown problems.
Moreover, epidemiological research suggests that
psychological factors, stress and undesirable social circumstances play
an important role in the occurrence of various cardiovascular diseases
[11,12] and are considered major risk factors for coronary heart
disease. The coronary-prone behavior pattern, called type A, that was
originally described by Friedman & Rosenman [13] in the late 1950’s,
has been considered a clinically derived behavioral syndrome
characterized by competitive drive, time urgency, hostility, and strong
job involvement. Characteristics as anger or aggression of a group of
patients have been demonstrated to be important factors for
cardiovascular and cerebrovascular disease [14] and
to be related to carotid atherosclerosis, while depression was
associated with endothelial dysfunction in diabetic patients
[15], predicts incident coronary artery disease and worsens its
prognosis [16-19], and anxiety is considered an independent
risk factor for incident coronary artery disease, for cardiac
mortality following acute myocardial infarction and cardiac
events [20,21]. In addition, there are different lifestyle behaviors
considered risk factors for coronary artery disease, as they
promote atherosclerosis and cardiac events, including unhealthy
diet, physical inactivity, smoking, obesity and sexual activity that
are related to emotional status and experience of chronic stress
[22].
As reported above, the relationship among cardiovascular
risk factors, atherosclerosis and cardio-cerebrovascular disease
occurrence appears a complex and intriguing issue not yet
completely and fully disentangled. The relationship between
psychological (stress, anxiety, depression, etc.) and behavioral
(over or unhealthy eating, obesity, smoke, physical inactivity,
sexual activity reduction/ lack and related diseases such as
hypertension, diabetes and dyslipidemia) factors is one of the
interesting issues that we try to deal with in the present paper
changing perspective to approach the several aspects and to look
at them from a different point of view.
We are convinced, from a wide literature and daily practice,
that the four pillars of good health, related to the individual’s
lifestyle and depending on his behavior, are:
- No Smoking
- Eating little
- Walking so much
- Sex a lot
What usually occurs today is that smokers are still too many,
over and unhealthy eating is widely spread and, consequently,
obesity is highly present in general population, only less than
50% of adult people practice regular physical activity and sexual
activity is influenced by several problems such as biological,
psychological, social, economic, political, cultural, ethical, legal,
historical, religious, and spiritual factors; but also by violence
against women, false beliefs and few knowledge’s and medical
like infections, organic dysfunctions, delivery complications [23].
For the latter, the report concludes: “Sexual and reproductive
health is fundamental to the social and economic development of
communities and nations, and a key component of an equitable
society a vital contribution to making the world a fairer place”
[23]. All of them are related to person’s psychological factors,
behavior and life style.
Within this context, we note that although cardiologists are
accustomed to managing lifestyle behaviors such as overeating,
obesity, smoking and physical inactivity, they are less likely to
assess and treat psychosocial risk factors, perhaps because of
their limited time, interest or familiarity with effective strategies
and recommendations [24] or because a systematic review,
based on few studies, refers that risk assessment, combined with
counseling, is associated with favorable but modest changes
in patient knowledge and intention to change and in provider
prescribing behavior and risk factor control [25].
For instance, regarding physical activity, only 47% of primary
care physicians include an exercise history as part of their initial
examination, whereas13% of patients report physicians giving
advice about exercise and physically active physicians are more
likely to discuss exercise with their patients [26-28]. But the
main issue of this situation is that the four pillars of good healthy
are widely influenced by psychological and behavioral factors in
the daily life by modifying the capability to adequately manage
the relationship with either the inside self emotions and feelings
or the outside, people and events included. More attention
should be paid to study all these aspects.
The individual may be summarily defined as a complex
organization in which neural, hormonal, cellular, and genetic
mechanisms are strictly related to social behaviors whose main
task is to help the organism to survive, reproduce, and care for
offspring sufficiently long that they too reproduced [25]. This
means that neuro hormonal structure of individual is related to
psycho behavioral one and that both influence one to each other
[29]. There exisists a wide literature reported in an interesting
review [30] that lists the numerous examples of reciprocal
influence of neuro hormonal and psycho behavioral structures.
In an interesting paper Rozanski et al. [24] consider three
psychological components that may be central to developing
emotional and coping flexibility: Vitality, Emotional Competence
and Positive response mechanisms. Vitality reflects the presence
of energy and enthusiasm and a sense of aliveness [31]; it is
characterized by two positive emotions, joy and interest, it is
fueled by both a sense of purpose and a sense of self-worth and
connotes a sense of positive excitement [24] and attitude.
Vitality promotes two adaptive responses (which may in turn
positively influence vitality itself): the development of various
positive response mechanisms (such as patience, discipline,
impulse control, strong social support, positive coping skills,
optimism) and emotional competence, that represents the ability
to regulate emotions across a range of situations [32], important
trait termed “emotional flexibility,” [33]. Briefly, a strong sense
of purpose coupled with a sense of self-worth derive benefit in
terms of a greater sense of vitality; this provides energy needed
to develop and mantain greater emotional competence and positive response mechanisms that in turn provide a stabilizing
force for maintaining a sense of vitality [24].
All this process well represents the individual’s relationship
(balance) between inner and outer and between neuro
hormonal and psycho behavioral structures. When several
factors negatively affect the structures the relationship is
unbalanced and anxiety, depression, stress, affective disorders
and psychological instability arise and grow up, evoking central
responses that cause multiple peripheral adverse effects such as
endothelial dysfunction, insulin resistance, obesity, hypertension,
inflammation, platelet activation, somatic symptoms [24]. It
is evident that stress as a complex of several psychological
situations, is the effect of multiple long acting factors that
progressively determine unbalancing of neuro hormonal and
psycho behavioral structures reducing the sense of purpose
and the sense of self-worth negatively modifying vitality,
emotional competence and positive response mechanisms and
consequenlty reinforcing cardiovascular risk factors.
“When you change the way you look at things, the things you
look at will change” is one of the quotes from Wayne W Dryer,psychologist and philosopher [34]. This is very useful to do
when the situation and thinking become temporarily intriguing
and complex and the solutions to problems are confused and
bleary. It is also useful when it is necessary to look at problems
from a different point of view in order to find more or better
solutions or the best one or when a new way to cope situations
and problems is needed to give suitable answers and acceptable
explanations to complicated and complex questions even if
they concerns acquired and apparently established issues.
Concerning the behavioral risk factors and according with that
reported above it is important to experiment a new point of view
orienting the attention towards person’s perception of them
self, his behavior and his inner/outer relationship unbalance
[35]. This means that it is necessary to take into account that all
acquired risk factors are a consequence of a bad relationship that
persons have, either with themselves (inner) or with the others
(outer), but it is also important to know what there is behind the
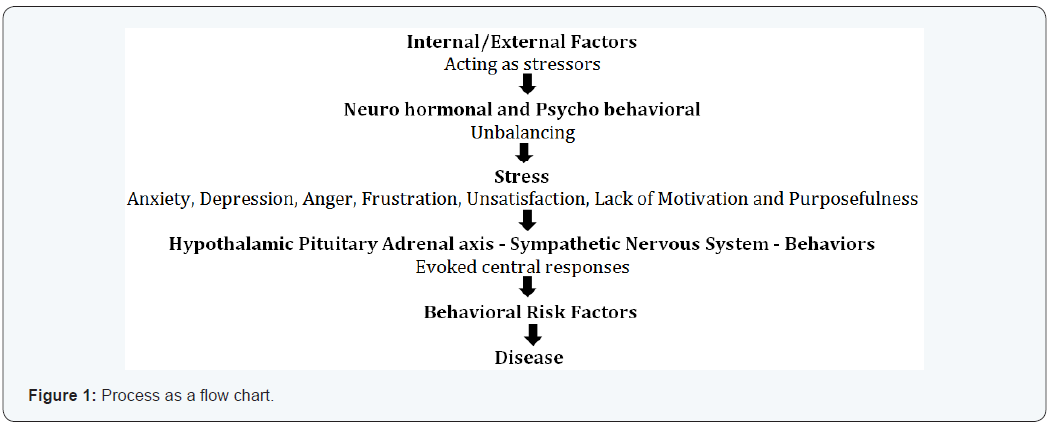
behavioral unbalancing [35]. We may hypothesize the following
process: (Figure 1) where several factors disturb along the time
the neuro hormonal and psycho behavioral balance provoking
stress; this induces multiple adverse peripheral effects related to
behavioral risk factors and then the onset of the disease.
In the light of this process we should look at problem paying
more attention to the persons (subjects or preclinical patients),
striving to understand what there is behind them that pushes to
unsuitable and deleterious lifestyle. Hippocrates wrote that “it
could not be possible to know medical practice for those who do
not know who and what is man; this is what must be understood
by those who shall take correctly care of men; if common man’s
comprehension will be missed… also reality will be missed.”
Investigators and clinical practitioners pay great attention to the
disease; a large literature exists considering cardiovascular risk
factors and their potential effect on disease onset [35]. However,
at the same time, literature is stingy in considering, for example,
that smoke, stress, obesity and alimentary disorders are not
the cause of something but rather the effect of an incorrect and inappropriate interpretation and management of relationships
that persons establish with those.
A different approach to behavioral risk factors should be
experimented orienting the attention towards what there
is behind their onset. A statement from the World Health
Organization (WHO) asserted that: “it is impossible to change
social values and health behavior without creating the
necessary atmosphere and condition” [36]. The strong and
robust relationship between psycho behavioral risk factors
and coronary artery disease suggests that cardiologists and
physicians in general need to be proactive in addressing this
important aspect of patient care [25]. Querying patients about
psychosocial risk factors conveys the message that these factors are important and relevant to providing optimal care. Screening
has been suggested using structured interviews or validated
questionnaires. The proposal is to obtain within the medical
history and assessment of the patient additional information
about psychosocial risk factors through questions regarding
emotional factors, such as depression, anxiety, and anger;
chronic stressors, such as work strain and home stress; and
somatic complaints that maybe stress-related, such as fatigue
and disrupted sleep [25].
We think that during the patient assessment questions should
be addressed deeply to find out what there is behind stress
and anxiety and which factors provoke the psycho behavioral
distress; more attention should be paid to the patient’s neuro
hormonal and psycho behavioral profile to understand better
the level of factor stressors, what is disturbing the patient
and what is linked to risk factors [35]. Many post myocardial
infarction or post heart surgery patients usually come daily to
our cardiology offices asking in many different ways, and deeply
convinced, to help them to quit smoking, to reduce weight, how
they can change their deleterious lifestyle; we cannot dismiss
patients with few hasty words. We must take care of their
psyco behavioral problems trying to identify and understand
the distress stressor factors and helping him to remove them.
The role of the cardiologist is important by exploring various
ways for effective clinical involvement and also by managing
these situations; in particular complicated cases, the specific
involvement of other specialists is recommended [37-39].
In our daily experience with patients’ problems we use,
with positive results in the majority of them, an approach in
four phases during a weekly counseling with a single patient.
The first phase aims to establish a relationship in empathy; the
second phases aims to help the patient to look at behind of things
and events, to look for into his past history and tell it; the third
phase has the aim to guide patients to realize what of his history
is disturbing or not and help him in his decision to remove them;
the final phase is used to reinforce patient’s resilience in order
to help him to find and appropriate use all the capabilities he
has put aside. During counseling, information on risk factors,
cardiovascular diseases, relationship among neuro hormonal
structure and function, behavior and cardiovascular apparatus
are given.
The final objective is to help the patient to recognize his own
problems, to help him to look at things from a different point
of view, to give him the necessary information to better manage
his disturbing factors and to help him to recover the emotional
energy and the positive sense of purpose and self worth: in few
words to reappropriate of himself, improve his lifestyle and look
at the future in a better way.
For more articles in Open Access Journal of Cardiology & Cardiovascular
Therapy please
click on:
https://juniperpublishers.com/jocct/index.php
https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment