Zero Percent Inappropriate Rates for Percutaneous Coronary Intervention are Achievable and Sustainable at One Year with a Multifaceted Quality Improvement Initiative-Juniper Publishers
Juniper Publishers-Journal of Cardiology
Abstract
Introduction: Appropriate Use
Criteria Scores for percutaneous intervention (AUC-PCI) are being used
to evaluate appropriateness of procedures performed by hospitals and
interventional cardiologists. Effective strategies for improving AUC-PCI
scores are needed.
Methods: We reviewed all
inappropriate for one year. Multiple interventions targeting the root
causes were implemented. We then evaluated the subsequent percentage
change for AUC scores, prior stress imaging, non-obstructive disease and
PCI volume.
Results: From 2012 Quarter 2-
2013 Quarter 1 (2012Q2-2013Q1) the inappropriate PCI rate was 1.7%;
Following the intervention, there were 0.0% inappropriate PCI for one
year. PCI volume increased by 5.35%; stress testing increased by 5.1%
and the rate of non-obstructive disease increased by 1.5%.
Conclusion: Our experience
demonstrates that 0.0% inappropriate PCI rates are not only achievable,
but can be sustained for one year. Secondarily, there was an increase in
stress testing and PCI volume without a change in the rate of
non-obstructive disease.
Abbreviations: AUC-PCI:
Appropriate Use Criteria Scores for Percutaneous Intervention; PCI:
Percutaneous Coronary Intervention; NCDR: National Cardiovascular Data
Registry; ACS: Acute Coronary Syndrome; SCAI-QIT: Society for Cardiac
Angiography and Interventions Quality Improvement Toolkit; CCS: Canadian
Cardiovascular Society; CABG: Coronary Artery Bypass Grafting; EMR:
Electronic Medical Record
Introduction
With the realization that overutilization of medical
services is a critical economic and public health concern, numerous
initiatives have been developed to address the problem. Due to its
widespread use, reducing the frequency of Percutaneous Coronary
Intervention (PCI) has been suggested as a goal [1]. The American
College of Cardiology has been supportive of efforts to reduce
overutilization of PCI in situations where there is limited evidence of
benefit. The Appropriate Use Criteria for percutaneous coronary
intervention (AUC-PCI) were released in 2009 and revised in 2012 to
guide clinical decisions [2]. To support utilization of AUC-PCI as a
quality metric, the National Cardiovascular Data Registry (NCDR)
provides AUC-PCI scores in benchmarked feedback reporting. Both private
and public scrutiny has caused AUC-PCI to quickly become an important
performance measure [1,3-5].
The 2012 AUC-PCI guideline divides indications into
three primary categories: Appropriate, Uncertain and Inappropriate. The
NCDR registry institutional outcomes report benchmarks the percentage of
each category relative to other institutions and all registry patients.
Reports are provided for all PCI patients, those with acute coronary
syndrome (ACS) and those without ACS (Non-ACS).
There are numerous challenges to improving AUC
scores. Foremost are the multiple potential causes. These include
documentation deficiencies, errors in data abstraction and variability
in clinical practice [6-8]. To achieve rapid improvement, we implemented
multiple interventions in parallel. This contrast with the traditional
cyclic model of performance improvement where the problem is identified,
a single intervention is planned, implemented and the results analyzed
prior to planning the next intervention.
Methods
To identify causes for inappropriate PCIs specific to our
institution, the NCDR individual fallout reporting feature was
utilized to identify all inappropriate cases for the second quarter
of 2012 through the first quarter of 2013(2012Q2-2013Q1).
The project physician lead (L. Box) reviewed all relevant
documentation. The root cause was identified and entered into
an excel spreadsheet. To develop interventions, we reviewed
recommendations from the Society for Cardiac Angiography and
Interventions Quality Improvement Toolkit (SCAI-QIT) webinar
“Navigating the New 2012 Revascularization Appropriate Use
Criteria” [9], presentations [10], the NCDR quality improvement
for Institutions website and the Accreditation for Cardiovascular
Excellence Cath/PCI standards [11].
Additional solutions were identified through discussion
with all involved providers. The interventions were initiated
beginning in July 2013 and were fully operational by the end of
2013Q4. Presently there is no established standard rate of each
category (A, U and I). The NCDR registry provides reports the 50th
percentile and 90th percentile for all participants for comparison.
We therefore targeted the 90th percentile performance level as our
goal. To better understand the impact on practice patterns, we
pre-specified PCI volume, the rate of pre-procedure stress testing
and the rate of negative angiograms as metrics but without set targets.
A secondary review was conducted to evaluate the accuracy of
documentation specifically related to Non-ACS PCI. Documentation
related to the indication for all outpatient coronary angiograms
for 2013Q1 was reviewed. A determination of the validity of the
stated indication based on the supporting documentation was
made in each case. The key variables as entered into the Cath-PCI
registry were then checked against the documentation to confirm
that documentation and data abstraction was accurate.
Results
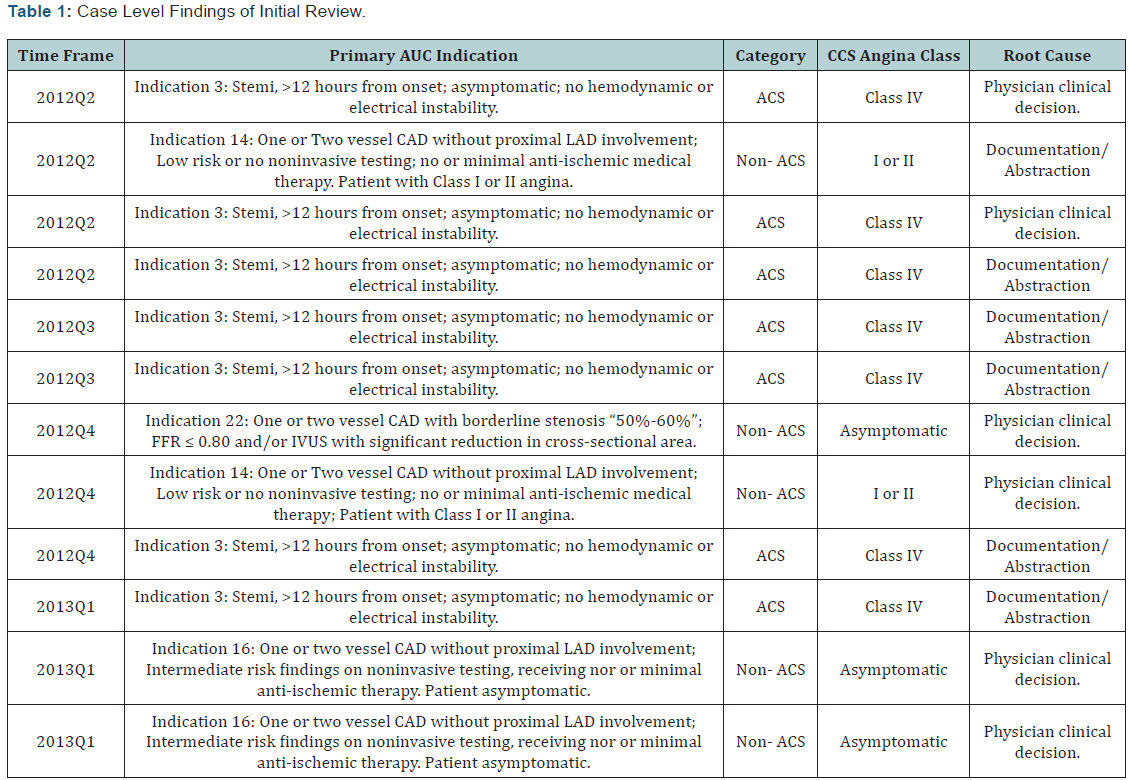
During 2012Q2-2013Q1, there were 12 cases scored I. Of
these, 7 were classified as ACS cases and 5 as Non-ACS. Guided by
the reviewer’s findings two primary causes were identified:
- Physician clinical decision
- Documentation and abstraction.
The second category reflected the difficulty with clearly
discerning the primary indication and clinical history at the time
of abstraction. In general problems with documentation also lead
to inaccurate data abstraction. Therefore, documentation and
abstraction problems were merged into a single cause. The initial
review findings are presented in (Table 1).
Guided by the chart review findings, we selected multiple
possible interventions for improving performance. These
interventions are listed in (Table 2). A recurring theme across
these interventions was improving documentation of the key
variables for determination of AUC: the Canadian Cardiovascular
Society (CCS) Angina Classification, the number of anti-anginal
medications, noninvasive testing results with a risk estimate and
a prior history of coronary artery bypass grafting (CABG) [12].
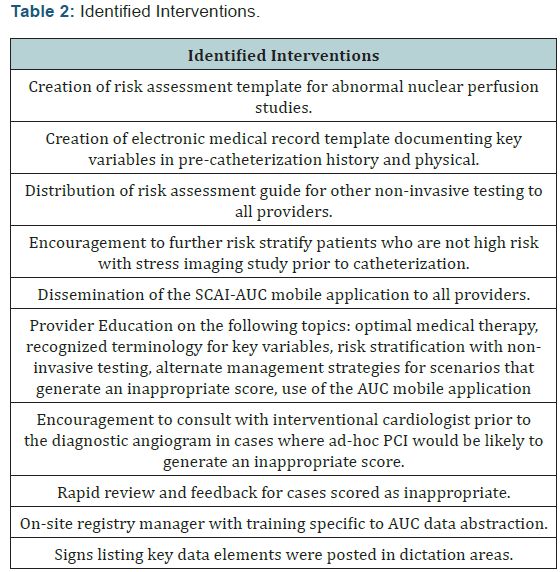
This was addressed not only with templates but also with
provider education regarding the data element definitions and
usage of proper terminology. Education on all interventions was
provided at conferences and physician meetings. To improve
the data abstraction process, a new position was created for an
onsite data registry manager. Previously, data abstraction was
done offsite. The position was filled by an RN with catheterization
laboratory experience (K. Dey). During orientation, the manager
was instructed on the abstraction process relevant to AUC. An
additional challenge identified in discussions was the hybrid
medical record system within our institution. The outpatient
setting utilized the EPIC electronic medical record (EMR) system
while the inpatient setting used paper charts with dictation. To
address this, signage regarding documentation of the key data
elements was placed in all inpatient areas frequently used by
physicians for dictation. All interventions were operational by the
close of 2013Q4 and the project was officially launched as part of
a divisional grand rounds presentation in December, 2013.
Data Analysis and Statistical Methods
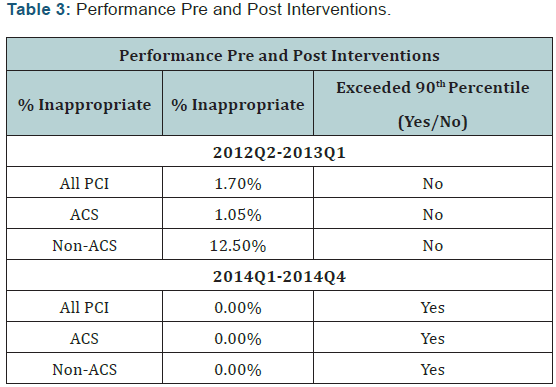
The results of our intervention were assessed by performance
on the NCDR Institutional Outcomes Report. Our focus was the
change in the percentage of inappropriate cases as well as the absolute goal of exceeding a 90th percentile performance level.
The additional metrics of volume, rate of stress testing and rate of
negative angiograms were reported as percentages without prespecified
targets.
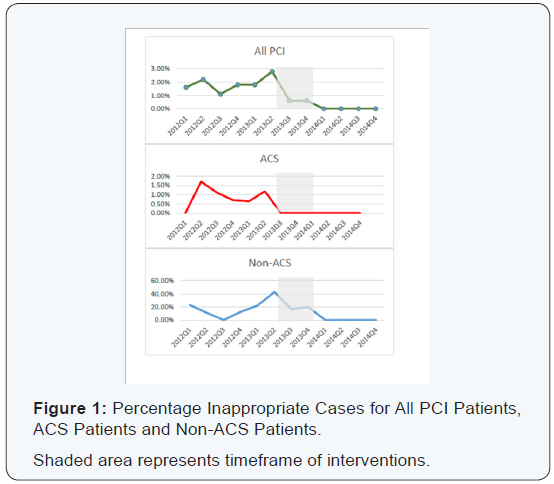
At one year, the rate of inappropriate interventions across
all categories was 0.00%, thus meeting the 90th percentile target
for each category at one full year post interventions (2014Q1-
2014Q4) (Table 3). During the implementation phase, 2013Q2
data had been submitted but was not available. The interventions
were in varying stages of implementation for 2013Q3-Q4. The
trajectory of improvement is presented in (Figure 1) depicting the
quarterly inappropriate score for 2012Q1-2014Q4. The number
of PCI procedures increased by 5.3%. The percentage of patients
with a stress or imaging study increased by 5.1%. The percentage
of patients with non-obstructive CAD increased by 1.5% (Table 3).
Secondary chart review of all elective cases demonstrated 100%
consistency of the stated indication for the procedure with the
supporting documentation. The documentation was also 100%
consistent with the data entry of key variables into the Cath-PCI
registry by the registry manager.
Recent works in this area show the new echocardiographic
methods such as strain rate and speckle tracking echocardiography
to enable easier, more objective and more accurate analysis of the
minimum, initial changes in the function of the right heart, which
will greatly contribute to an easier and more precise diagnosis
and improved treatment of heart diseases in children.
Discussion
Since the introduction of PCI AUC in 2009, hospitals and
physicians have struggled with implementation. One challenge
is the lack of an acceptable threshold. It is not intended that
AUC scores be 100% Appropriate or 0% Inappropriate [12]. At
the hospital level, AUC scores have been shown to have a wide
variation [13,14]. The NCDR registry allows benchmarking
against other institutions with a reported inappropriate 50th
percentile for ACS of 0% and Non-ACS of 13.5% for the 2014Q1-
Q4. Patient level analysis of NCDR data for July 1, 2009 and
September 20, 2010 demonstrated inappropriate ratings of 1.1%
for ACS and 11.6% for Non-ACS [15]. Data from other registries
have found similar rates. Analysis of PCIs performed in the state of
Washington during 2010 found inappropriate ratings 1% for ACS
and 17% for Non-ACS [13]. Examination of the New York State
PCI registry found 14% of Non-ACS PCI scored inappropriate
[16]. In the highly controlled environment of the courage trial,
the numbers were much lower with retrospective analysis finding
only 5.1% of interventions inappropriate [17].
Our experience demonstrates that a 0% rate of inappropriate
is both achievable and sustainable. There have been prior reports
of successful quality improvement initiatives for AUC scores.
Utilization of the SCAI AUC application was reported by both
Chen & Jackson [18,19] as an effective tool for improving AUC
scores. Provider education has also been reported as effective
[20]. A multifaceted approach was described by Beauvallet et al.
& Wong et al. [6,21] but they did not achieve the same degree of
improvement nor did they report sustained improvement over
one year.
Our efforts included the active involvement of a physician
lead and strong engagement of all interventional cardiologists
within our institution. Many potentially inappropriate PCIs were
avoided by informal consultations prior to angiography. Timely
communication between the registry manager and providers
through feedback reports rapidly improved both documentation
and abstraction. Having a dedicated registry manager on site
facilitated this process.
Most of our interventions were voluntary. However, the use
of templates for reporting stress test risk results and for preprocedure
documentation of key variables were adopted by the
division as mandatory. These requirements are likely to have the
greatest impact on AUC performance improvement [9-13]. Use of
the SCAI AUC application was optional but it was adopted by many
providers. The educational intervention addressed variations
in clinical management leading to inappropriate scores. Group
discussion of alternative management strategies for common
inappropriate scenarios reinforced didactic education and
increased provider comfort.
There were likely other factors beyond the
interventions
contributing to the low inappropriate rate. It has been reported
that regional practice patterns of lower utilization predicts lower
scores [22]. In fact this study was conducted in an area with lower
rates of PCI utilization. The Dartmouth Atlas reported 4.4 inpatient
PCI procedures per 1000 medicare beneficiaries for the state of
Idaho in 2012, which is at the 10th percentile [23]. Our lower than
average rate of negative angiograms (Table 3), higher symptom
burden, greater use of two anti-anginal agents and percentage
of high risk stress tests suggests a conservative management
approach across providers. In particular, our negative angiogram
rate suggests good patient selection [24].
Critics of AUC have suggested that procedures based on sound
clinical judgment may be deemed inappropriate by AUC criteria
[25]. This raises the concern that patients might be denied needed
care due to concern over performing an inappropriate procedure.
This was not a clinical study and therefore we cannot exclude this
possibility, however, there were no anecdotal reports to support
this concern. Analysis of the courage trial data suggests that such
events would be infrequent [17]. A possible interpretation of our
success is that documentation did not accurately reflect the true
clinical scenario. Our secondary analysis of all cases for 2013Q1
argues against this possibility.
To verify the validity of this review, the documentation and
abstraction process was also discussed with the NCDR staff and it
was felt that our methods were sound. Physicians were educated
on utilization of terminology that was consistent with the NCDR
data dictionary, but were explicitly instructed against intentionally
misrepresenting the clinical facts to avoid inappropriate scores.
There has been widespread speculation that overutilization of PCI
is driven in part by economic concerns and that implementation
of AUC would decrease the number of PCIs being performed [8].
During this initiative, PCI volumes actually increased. While this
may have been due to multiple factors, it certainly does not support
the claim that AUC will reduce the number of interventions.
Conclusion
Given that providers were encouraged to increase utilization
of noninvasive testing prior to coronary angiography, it is not
surprising that the percentage of noninvasive testing increased.
Interestingly, this did not change the frequency of nonobstructive
disease found at the time of angiography. This could
be interpreted both as a sign that needed care was still being
delivered or alternatively, that the utility of noninvasive testing
in the evaluation of ischemic coronary artery disease is lower
than current perception. The most likely interpretation is that
given the conservative practice style already in existence within
our group, the increase in stress testing had a minimal impact.
It does raise the concern that broad implementation of AUC may
actually increase cost while not improving care beyond what can
be achieved with sound clinical judgment.
LimitationsLimitations of this study include the study design, which was a single center observational study. We cannot make any conclusive statements regarding the clinical effects of our interventions. Future studies regarding the clinical impact of very low inappropriate AUC scores need to be conducted in a prospective, randomized trial. However, given the current available evidence, we do believe it is reasonable for institutions to target the lowest inappropriate AUC scores possible. This report provides an overview of a successful multifaceted approach to reach this goal.



Comments
Post a Comment