Heart Failure-Juniper Publishers
Heart failure (HF) is a complex clinical syndrome
that can result from any structural or functional cardiac disorder that
impairs the ability of the ventricle to fill with or eject blood. The
cardinal manifestations of HF are dyspnea and fatigue, which may limit
exercise tolerance, and fluid retention, which may lead to pulmonary
congestion and peripheral edema [1]. Atrial fibrillation (AF) is the
most common arrhythmia in clinical practice, accounting for
approximately one third of admissions resulting from cardiac rhythm
disturbances [2].
Introduction
The association between AF and heart failure was
appreciated almost a century ago [3]; Paul Dudley White noted, “Since
auricular fibrillation so often complicates very serious heart disease,
its occurrence may precipitate heart failure or even death, unless
successful therapy is quickly instituted [4]. The reported prevalence of
AF in modern heart failure series ranges from 13% to 27% [5-9].
Moreover, the prevalence of AF in patients with heart failure increased
in parallel with the severity of the disease, ranging from 5% in
patients with mild to 10% to 26% among patients with moderate up to 50%
in patients with severe heart failure [10].
The impact of right ventricular function on survival
in patients with advanced HF has been underlined by studies showing that
left ventricular function loses its prognostic value in patients with
an ejection fraction of less than 25%, while a preserved right
ventricular ejection fraction proved to be predictive for exercise
capacity and survival even in advanced HF. These studies have supported
the need for a method which allows a simple and rapid evaluation of
right ventricular function [11].
Peak systolic tricuspid annular velocity determined
by Doppler tissue imaging is a simple parameter with reasonable
correlation to right ventricular ejection fraction (EF). A low peak
systolic tricuspid annular velocity proved to have high predictive
accuracy for right ventricular dysfunction (EF<45%) determined by
radionuclide ventriculography [12].
Methods
Our study was a prospective analysis of 40
consecutive patients who were admitted to Assiut University Hospital
with chronic AF and impaired LV systolic function (EF≤45%). Patients
with severe comorbid conditions, decreased life expectancy from other
non-cardiac causes eg. Malignancies, primary lung diseases, or primary
tricuspid valve disease were excluded from the study. The protocol was
accepted by the medical ethics in human investigation committee of our
institution.
All patients were subjected to full history taking,
complete general and cardiac examination, and twelve leads ECG.
Conventional echocardiography was done for all the study population at
the beginning of the study. Assessment of cardiac dimensions and
functions was done where left atrial (LA) and LV dimensions were
measured using M-Mode in the parasternal long axis view. LV systolic
functions were assessed using 2D Simpsons’s method from both apical
2-chambers and apical 4-chambers views, to measure EDV, ESV, and EF%.
Diastolic functions were evaluated by transmitral flow where total
diastolic filling time, and E wave deceleration time were assessed.
Right ventricular diameter was measured by M-Mode of paratsternal short
axis viewat the level of papillary muscles. RVEF was assessed by
Simpson’s method in apical four chamber and apical two chamber views.
PWTDI of TVA was recorded from apical 4-chamber view
where tricuspid annular systolic and diastolic velocities were
acquired at the junction of the right ventricular free wall and the
anterior leaflet of the tricuspid valve. Lateral S velocity, Lateral
E velocity, Time to Lateral S, Time to Lateral E, Medial S velocity
and Medial E velocity were recorded.
The patients were followed up for six months for
development of clinical adverse events in the form of:
readmission with heart failure, increased diuretic use, and
thromboembolic manifestations. The primary end point was
cardiac death. Correlations were done between the occurrence
of cardiovascular events and conventional echocardiographic
parameters including LA diameter, LVEDD, LVEF and RVEF.
Events were correlated to tricuspid annulus pulsed wave tissue
Doppler findings including Lateral S velocity, Lateral E velocity,
Time to Lateral S, Time to Lateal E, Medial S velocity and Medial
E velocity.
Statistical Analysis
Data were analyzed by statistical package for the social
sciences (SPSS, version 16.0). The ranges, means, standard
deviations were calculated for interval and ordinal variables
and the frequencies and percentages for categorical variables.
Univariate correlations were estimated between the occurrence
of cardiovascular events and conventional echocardiographic
parameters including LA diameter, LVEDD, LVEF and RVEF using
Pearson correlation coefficient (r). Events were also correlated
to tricuspid annulus pulsed wave tissue Doppler findings
including Lateral S velocity, Lateral E velocity, Time to Lateral S,
Time to Lateal E, Medial S velocity and Medial E velocity.
The univariate correlation between conventional and PWTDI
parameters of TVA and all included variables was assessed by
Pearson correlation coefficient (r) which were calculated to
detect the strength and significance of association between a
pair of variables measured on the interval, ordinal, dichotomous
scale in each patient group separately. The probability (P value)
less than 0.05 was taken as the limit of statistical significance.
Results
In this study, the patient’s mean age was 49.03 ± 12.19 years
(ranging from 29 – 80 years). Number of males was 22 (55.0%)
and number of females was 18 (45.0%).
Echocardiographic Findings
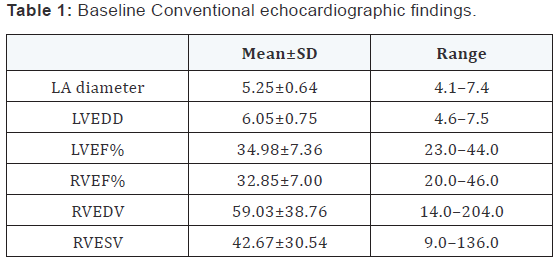
Baseline Conventional Echocardiographic findings
(Table 1): We found that mean LA diameter was 5.25 ± 0.64 cm
(ranging from 4.1 – 7.4 cm), and mean LVEDD was 6.05 ± 0.75cm
(ranging from 4.6 – 7.5cm). Also we found that mean LVEF was
34.98 ± 7.36 % (ranging from 23.0 – 44.0 %), and mean RVEF
was 32.85 ± 7.00% (ranging from 20.0 – 46.0%). RVEDV was
59.03 ± 38.76 (ranging from 14.0 – 204.0 ml), and RVESV was
42.67 ± 30.54 (ranging from 9.0 – 136.0 ml).
Baseline Tricuspid Annulus pulsed wave tissue Doppler
findings: In our study we found that the mean lateral S velocity
was 8.46 ± 1.60 cm/sec (ranging from 5.8 – 13.8 cm/sec), while
the mean lateral E velocity was 11.86 ± 2.37cm/sec (7.1 – 16.7c
m/sec), and mean Time to Lateral S was 184.98 ± 29.14 m/sec
(ranging from 127.0 – 265.0 m/sec).
Also we found that the mean Time to Lateral E was 452.08 ±
49.75 m/sec (ranging from 360.0 – 545.0 m/sec), and the mean
Medial S velocity was 5.40 ± 1.07 cm/sec (ranging from 3.3 –
7.9cm/sec), and finally the mean Medial E velocity was 6.93 ±
2.24 cm/sec (ranging from 2.7 – 13.6 cm/sec) (Table 2).

Follow-up
Patients included in this study were Followed-up for six
months for occurrence of cardiovascular events in the form of
death, admission with HF, increase of the diuretics dose, and
thromboembolic manifestations.
During the follow-up period, 10 patients reached the primary
end point {10 admissions by HF (including three deaths), 6 cases
increased the dose of diuretics (were admitted by HF), and one
case of thrombo embolic manifestation (died)}.
Correlations were done between occurrence of events
and echocardiographic findings of the patients (including
conventional and tricuspid annulus pulsed wave tissue Doppler).
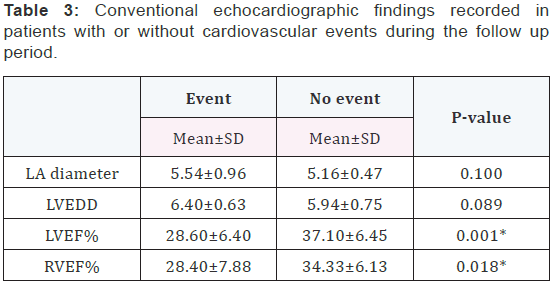
Conventional echocardiography with or without events: After the follow-up period, there was significant relation as
regard both LVEF (with mean 28.60 ± 6.40% in patients with
events, and 37.10 ± 6.45 % in patients without events, p=0.001)
and RVEF (with mean 28.40 ± 7.88% in patients with events, and
34.33 ± 6.13% in patients without events, p=0.018 ) (Table 3).
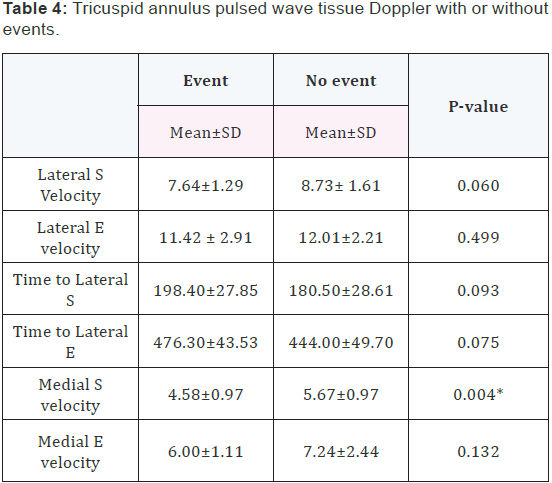
Tricuspid annulus pulsed wave tissue Doppler with or
without events: There was significant relation only between
Medial S velocity and occurrence of cardiovascular events (with
mean 4.58 ± 0.97 cm/sec in patients with events, and 5.67 ± 0.97
cm/sec in patients without events, p=0.004) (Table 4) (Figure
1). There was insignificant relation between the occurrence of
cardiovascular events and Lateral S Velocity (with mean 7.64 ±
1.29 cm/sec in patients with events, and 8.73 ± 1.61 cm/sec in
patients without events, p=0.060). Also, there was insignificant
relation between occurrence of cardiovascular events and
Lateral E velocity (with mean 11.42 ± 2.91 cm/sec in patients
with events, and 12.01 ± 2.21 cm/sec in patients without events,
p=0.499), and with Time to Lateral S (with mean 198.40 ±
27.85msec in patients with events, and 180.50 ± 28.61 m/sec
in patients without events, p=0.093). Time to Lateral E showed
insignificant relation with the occurrence of events (with mean
476.30 ± 43.53 m/sec in patients with events, and 444.00 ±
49.70 m/sec in patients without events, p=0.075). And finally
Medial E velocity also showed insignificant relation with the
occurrence of events (with mean 6.00 ± 1.11 cm/sec in patients
with events, and 7.24 ± 2.44 cm/sec in patients without events,
p=0.132) (Table 4).

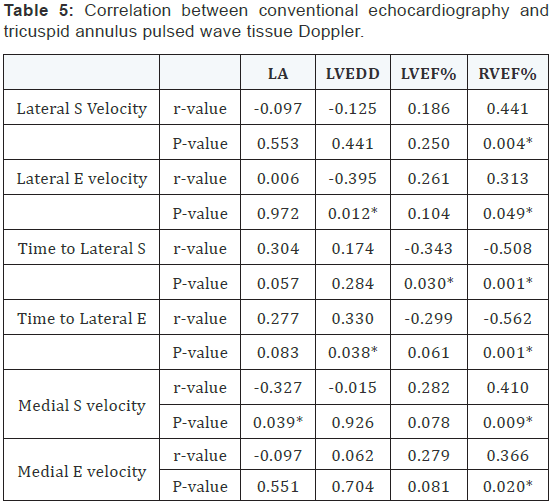
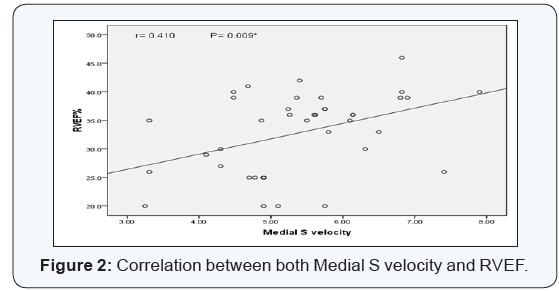
Correlation between conventional echocardiography
and tricuspid annulus pulsed wave tissue Doppler: There
was significant correlations between RVEF and some of the DTI
parameters of the tricuspid annulus (Lateral S peak velocity with
p=0.004 and correlation coefficient (r) =0.441, Lateral E peak
velocity with p=0.049 and correlation coefficient (r) =0.313,
Time to lateral S with p=0.001 and correlation coefficient
(r) =-0.508, Time to lateral E with p=0.001 and correlation
coefficient (r) = -0.562, Medial S peak velocity with p=0.009 and
correlation coefficient (r) = 0.410, and Medial E peak velocity
with p=0.020 and correlation coefficient (r) = 0.366). Also there
was significant correlations between LVEF and time to lateral S
with p=0.030 and correlation coefficient (r) =-0.343 (Table 5).
LVEDD was significantly correlated with Lateral E peak velocity
with p=0.012 and correlation coefficient (r) = 0.395, and Time
to lateral E with p=0.038and correlation coefficient (r) = 0.330.
LA diameter was significantly correlated with Medial S velocity
with p=0.039 and correlation coefficient (r) = -0.327 (Table 5)
(Figure 2).
Discussion
The assessment of prognosis in patients with AF has been
performed in the clinical course of HF [13,14]. AF is believed to
share pathophysiologic associations with hypertension and HF,
although no definite etiology has been determined. Regarding the
outcomes of HF, the concomitant presence of AF could be used
to identify high-risk patients to prevent subsequent hospital
admissions. In patients with AF, left ventricular (LV) diastolic
or systolic dysfunction is frequently encountered, leading to left
atrial (LA) enlargement and pressure elevation.
The electromechanical features of AF may impair ventricular
filling and cause irregular contraction with poor ventricular
rate control, resulting in a cardiomyopathy that is common in
the left ventricle but may also be seen in right ventricle [15-
17]. Consequently, AF commonly has adverse hemodynamic
effects on both left and right ventricles, causing right ventricular
(RV) dysfunction or HF. RV function is also considered to be
an independent predictor of clinical events in HF, irrespective
of LV functional severity [18,19]. Furthermore, Doppler tissue
imaging (DTI) of the tricuspid valve (TV) annulus has been
found to provide information about RV longitudinal function in
previous studies [20]. Interestingly, systolic myocardial velocity
as determined from the TV annulus could be a significant
predictor of RV function and has proven to be a useful index in
the prognosis of RV infarction [21].
However, few studies in the literature have examined DTI
of the TV annulus in patients having HF with AF, although DTI
is easily used for LV evaluation. In addition, patients with nonsinus
rhythms such as AF have been usually excluded from
echocardiographic studies. Despite the prognostic significance
of AF in terms of HF, AF has not shown a consistent impact
for prognosis in patients with HF, but rather, its impact might
be dependent on the severity of HF [22]. Importantly, the
association of TV DTI with AF has not been evaluated or focused
in studies of HF.
Therefore, we hypothesized that TV DTI would be as
important as mitral valve (MV) DTI for clinical outcomes,
particularly in the setting of clinical AF. The goals of the present
study were to quantify RV dysfunction and to assess prognostic
value of tricuspid annulus tissue Doppler velocity in heart failure
with atrial fibrillation.
In our study we used different parameters to assess RV
dysfunctions as a predictive method to assess the prognosis
of heart failure with atrial fibrillation. Our study includes 40
cases of heart failure (with ejection fraction less than 45%) with
atrial fibrillation. We have done conventional echocardiography
and DTI study of the tricuspid annulus including lateral S
velocity, lateral E velocity, time to lateral S, time to lateral E,
medial S velocity and medial E velocity. The patients were
followed-up for 6 months for occurrence of cardiovascular
events. Relations were done between the cardiovascular events
occurred during the follow-up period and the echocardiographic
findings at the beginning of the study. Moreover, correlations
were done between the DTI of the TV and the conventional
echocardiographic findings according to the occurrence of the
cardiovascular events in the follow up period.
At the end of the study there were 3 deaths reported with
a percentage of 7.5%, 10 admissions with heart failure with a
percentage of 25%, 6 cases increased the dose of diuretics with
a percentage of 15%, and there was one case of cerebrovascular
stroke with a percentage of 2.5%. DTI of the tricuspid annulus
revealed that the lower medial S velocity, the more significant
relation with occurrence of cardiovascular events in the follow
up period (with mean 4.58 ± 0.97 cm/sec in patients with
events, and 5.67 ± 0.97 cm/sec in patients without events,
p=0.004). But there were no significant relation with occurrence
of cardiovascular events and the other parameters of RV DTI
including Lateral S, medial E and lateral E velocities. Those
results were with the agreement with Kim et al. [23] who
reported that most patients with left HF exhibit RV dysfunction,
evidenced by low tricuspid annular DTI velocities including
Medial S peak velocity. But we disagree with Kim et al. [23] in the
significance of the medial E and Lateral S velocities as predictive
of cardiovascular events [23].
We disagree in our study with Meluzin J et al. [24] as they
reported in their study that the peak systolic annular velocity
was significantly lower in patients with heart failure than the
healthy subjects (10.3 +/- 2.6 cm. s(-1) vs 15.5 +/- 2.6 cm/sec, P
< 0.001) [24]. In agreement with De Groote et al. who dedicated
that in patients with moderate heart failure, RVEF in addition to
the NYHA functional classification was an independent predictor
of survival and of major cardiac events [25]. We found significant
relation between the occurrence of cardiovascular events and
the lower the RVEF (with mean 28.40 ± 7.88% in patients with
events, and 34.33 ± 6.13% in patients without events, p=0.018).
In agreement with Solomon et al. [26] who dedicated that
LVEF is an important and powerful predictor of cardiovascular
outcomes, including all-cause mortality, cardiovascular
mortality, sudden death, heart failure–related death, fatal
or nonfatal MI, and heart failure hospitalization. Every 10%
reduction in ejection fraction below 45% was independently
associated with a 39% increased risk for all-cause mortality, with the most common events experienced being sudden
death and heart failure–related death [26]. We found in our
study a significant relation between reduction of LVEF and the
occurrence of cardiovascular events (with mean 28.60 ± 6.40%
in patients with events, and 37.10 ± 6.45 % in patients without
events, p=0.001).
In agreement with Kizer et al. [27] who reported in
their population-based cohort, LA diameter independently
predicted incident cardiovascular events after adjustment
for established clinical, echocardiographic, and inflammatory
risk factors [27]. We found in this study significant relation
between cardiovascular events and the LA diameter (with mean
5.54 ± 0.96 cm in patients with events, and 5.16 ± 0.47 cm in
patients without events, p=0.1). While in a study was done by
Tsang et al. [28] in 2005, said that Indexed LA volume is a more
robust cardiovascular risk marker than LA area or diameter
in patients who are in sinus rhythm; however, in patients with
AF, the predictive utility of LA size for future cardiovascular
events seemed unsatisfactory, regardless of the method of LA
quantitation [28].
In our study we made a correlation between the conventional
echocardiographic findings of the patients and the DTI study of
the tricuspid annulus, which revealed some positive correlations
in various parameters. There was significant correlation
between Time to lateral S and RVEF (with p=0.001 and
correlation coefficient (r) =-0.508), which is supported by the
study of Meluzin J et al [24]. Also Meluzin J et al. [24] reported
that there was a good correlation between systolic annular
velocity and right ventricular ejection fraction (r = 0.648, P
<0.001). A systolic annular velocity < 11.5 cm/sec predicted
right ventricular dysfunction (ejection fraction < 45%) with a
sensitivity of 90% and a specificity of 85% [24]. which supports
our study where we find a significant correlation between peak
systolic annular velocity lateral S and RVEF with p=0.004 and
correlation coefficient (r) =0.441.
In our study, there were various significant correlations
between RVEF and other tricuspid annulus DTI parameters
including Lateral E velocity, Time to lateral E, Medial S velocity,
and Medial E velocity. Lateral S velocity showed significant
correlation with LVEF with p=0.250 and correlation coefficient
(r) = 0.186. LVEDD was significantly correlated in this study with
two parameters, lateral E velocity and time to lateral E (p=0.012
correlation with coefficient (r) =-0.395, and p=0.038 with
correlation coefficient (r) = 0.330, respectively). LA diameter
was only significantly related to Medial S velocity with p=0.039
and correlation coefficient (r) = -0.327.
Conclusion
RV functions including RVEF and Doppler tissue imaging
)DTI( of tricuspid annulus can be a good predictor of
cardiovascular events and the prognosis of heart failure with
atrial fibrillation.



Comments
Post a Comment