Prehypertension: A Study in Youth-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Background: Youth of 18 to 20 year age achieve medical college admission through tough competition. Genotype, phenotype and environmental interactions that drive cardiovascular and other lifestyle diseases may be meaningfully recognized at such stage. Early detection of lifestyle disease and its determinants can guide timely interventions and correction toward prevention/reduction of morbidity and mortality.
Objective: Screening of first year male and female medical students for pre-hypertension and a study of family history, clinicodemographic and biochemical characteristics in comparison with normotensive peers.
Method: In a cross sectional study, 23 subjects (16 males and 7 females) in 18-20 year age range found to be prehypertensive upon screening were compared with 15 mached normotensive peers(10 males and 5 females). Familial, psychological behavioral, clinicodemographic and biochemical parameters were examined do define relevant associated trait of prehypertension.
Result: History of maternal hypertension was significant determinant of prehypertension. Dietary and physical activity profiles did not differ but psychologic morbidity was more prevalent in prehypertensives as opposed to the normotensives. Obesity and activation of sympathetic nervous system were particularly associated with prehypertension group. Hyperinsulinaemia and insulin resistance was significantly associated. Lipid profile and level of inflammatory marker homocystein did not significantly differ between prehypertensive group and the normotensive controls.
Conclusion: Family history, obesity, and psychological morbidity had higher association with state of prehypertension. Screening is early age is important to unravel prehypertension and metabolic syndrome, especially in subjects with family history of such disorders. Such subjects can be investigated for risk factors and monitored for disease progression. Timely institution of measures for weight reduction, lifestyle modification, dietetics etc, should avert disease progression and complications.
Keywords: Familial cardiovascular disease; Prehypertension; Metabolic syndrome; Resting heart rate; Homocystein
Introduction
Hypertension is major health concern with rising prevalence world over [1]. Hypertension constitutes 5% of total global disease burden and is implicated in 20% to 50% of all deaths [2]. Hypertension frequently in heres familial atherosclerosis risk [3]. Blood pressure elevation frequently originates in childhood [4]. Overweight and obesity are common risk factors for development of hypertension. Obesity associates increased sympathetic autonomic activity and increased vascular tone [5,6]. Fetal growth retardation, common among the Asians, results in epigenetic aberrations making the offspring vulnerable to develop metabolic syndrome at much younger age upon exposure to adverse environmental determinants as lifestyle and diet [7]. Cardiovascular risk rises continuously across the whole range of blood pressure elevation and underlies coronary heart disease, stroke and other vascular complications. Hypertension is singularly responsible for 1.9% of life years lost and 1.4% disability adjusted life years of global humanity on average [8].
Amid such scenario hypertension and its likelihood need early detection for timely preventive and therapeutic address to avert serious cardiovascular consequences. Medical students from the first year 2009 admission batch at MGM Medical College Navi Mumbai (India), were screened for aberrant blood pressure profiles. Detected prehypertensive profiles merit study of causal issues in the specific population. Clinical evidence so generated, should guide appropriate individualized and general approaches to prevention of hypertension and associated morbidities and mortality.
Subjects and Method
The study protocol involved interview, anthropometry and blood sampling, which was approved by superior research authority. Informed consent of the students was obtained prior to their inclusion in study. Physically handicapped subjects and those on any long term medication were excluded. Those giving history of suffering any illness within a month requiring suspension of routine activities for 3 days or longer were also excluded. Finally 90 subjects (48 males and 42 females) in 18 to 20 year age range were examined.
Resting blood pressure was recorded as per standard method [9], in sitting position after 5 minute rest by mercury sphygmomanometer in right hand, in the quiet clinical physiology room in the Physiology Department in morning between 9am to 10am. Further two measurements were taken at 5 minute intervals to compute average value as data. Students having systolic blood pressure above 120mm Hg to 139mm Hg and/or diastolic blood pressure above 80mm Hg to 89mm Hg were identified as prehypertensives. The hypertensive cutoff was 140/90mm Hg [9,10]. The examination yielded 16 males (33.3%) and 7 females (16.7%), exhibiting prehypertension range of blood pressure. These formed the prehypertensive study group. Control group of normotensives was chosen randomly by toss from the rest comprising 10 males and 5 females.
Detailed interview to elicit history of high blood pressure illness in mother/father or both was conducted. Anthropometric measurements (weight, height, waist and hip circumference) were performed using standardized techniques and the body mass index (BMI), was calculated as body weight in kg/ height in m2. All subjects were screened on a 6 point Centre of Epidemiological Studies Depression (CESD) questionnaire [11]. An assessment of anxiety on 5 point scale [12], was made by grading feeling of nervousness (i.e. never; occasionally; now and then; frequently; daily some time; most of the time). Frequency of exercise in a week was enquired. Using a 24 hour dietary recall, approximate daily calorie consumption was estimated using chronometer software (http/cron-o-meter.com), and % fraction of calories derived from saturated fat consumption was derived as relevant for Indian patients [13].
All participants were examined under fairly similar conditions of October and November. They were instructed to come without consuming coffee or tea and maintain activity as routine over the antecedent 24 hours. Systolic and diastolic blood pressure were measured a fresh, after the subjects have been seated quietly with back supported, feet on the floor and right arm supported for five minutes. Radial pulse rate was then counted in right hand for 30 seconds as per standard procedure [14].
Blood biochemistry tests included, fasting blood sugar, plasma insulin level, and lipid profile and homocystein level. Blood sugar and lipids were analyzed by central investigation lab of the college while insulin and homocystein analyses were outsourced from M/s Jariwala labs, Borivali, Mumbai. Glucose was estimated by glucose oxidase method and plasma lipids determined using enzymatic method. HDL-cholesterol measurement involved homogeneous colorimetric method. LDL- cholesterol was calculated using Friedwalds formula [15]. Serum insulin measurement was by radioimmunoassay technique [16] and homocystein by high performance liquid chromatography (HPLC) technique [17]. The serum separated within an hour of withdrawing blood was frozen at -20 °C and transported in dry ice for distant estimation.
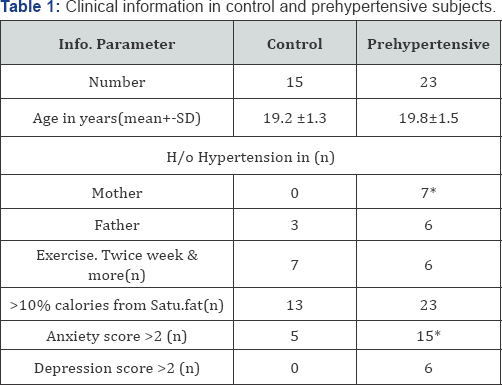
* P<0.05 (Chi square/Fishers Tests)
As shown in Table 1, prehypertensives have significant history of maternal hypertension while paternal history was indifferent from normotensive control. Neither exercise pattern nor dietary saturated fat consumption significantly differ between two groups. Higher anxiety and depression prevailed among the prehypertensives in contrast to controls.
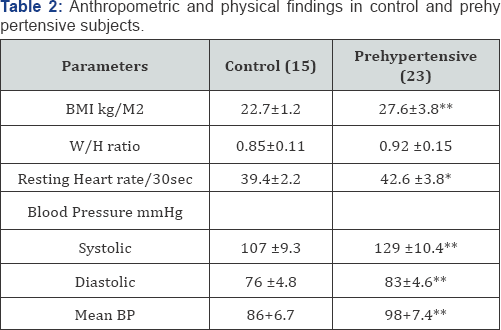
*P<0.01;** P<0.0001 (paired t test)
Table 2, shows significantly higher BMI and W/H ratios in the prehypertensives. The W/H ratio of prehypertensives was above the cut off for central obesity pattern. The systolic and diastolic blood pressures were obviously higher, even resting heart rates were significantly higher in prehypertensives.
Table 3 displays biochemical profiles. Although values of fasting blood glucose and serum homocystein were higher in prehypertensives than in controls, differences were not statistically significant. Fasting serum insulin levels were significantly raised in prehypertensives. This indicates relative insulin resistance among the prehypertensives.
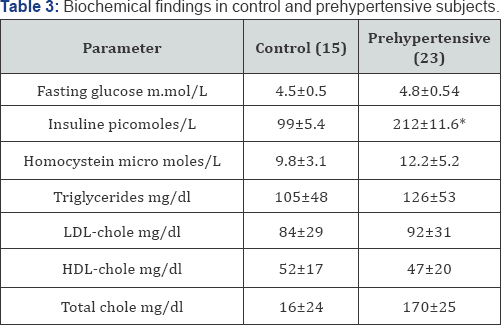
*P<0.0001 (paired t test
Discussion
Urbanization of lifestyle with nutrition transition that involves increased consumption of processed energy dense food are blamed for spread of lifestyle diseases as diabetes and hypertension [7-17]. Prehypertension as such, does not constitute disease but leads to two fold increase in risk of mortality due to coronary artery disease and cerebrovascular accidents [18]. Without lifestyle modification or pharmacologic intervention the prehypertensives are twice as likely to suffer hypertension in few years [19]. 34% to 46% population prevalence of prehypertension is reported in other societies [20-22]. Very different prevalence observed in present study may partly be accounted to the restricted age and socioeconomic group.
Family history of cardiovascular ailment encompasses genetic, biochemical and behavioral contexts and has shown influence on lipids [23], inflammatory markers [24] and haemostatic markers [25]. Individuals with family history of premature atherosclerosis are at higher risk of developing atherosclerosis [26]. Greater risk associated with maternal cardiovascular disease history, may reflect phenotypic evidence that birth weights affect subsequent hypertension [27], insulin resistance [28], and diabetes [29]. The complex mechanisms implied in family history warrant personalized elucidation to discover worthwhile targets for manipulation for disease prevention/reduction [30].
Dietary and physical activity perspectives play role in development of metabolic syndrome wherein, hypertension may be a component. Dietary and physical activity patterns did not differ between compared groups. The prehypertension group exhibited significantly higher prevalence of anxiety and depression that cause adverse biological impact leading to systemic inflammation, endothelial and platelet dysfunction. They also disturb sympathovagal balance leading to impaired protective vagal regulation and increased heart rate [31-33].
The average BMI among prehypertensive group, 27.6kg/ m2 is obesity range by Indian standards [34]. Frequent high W/H ratio is indicative of central obesity selectively associating prehypertension. The insulin levels are significantly higher in prehypertensive group as compared to control, suggesting insulin resistance.
Obesity associate increased sympathetic activity [5,6] and obese adolescents are at increased risk of developing hypertension in adulthood [35]. The findings are in agreement with reported association of insulin resistance in prehypertension [36]. Excess visceral fat reduces hepatic clearance of insulin resulting in Hyperinsulinaemia [37]. Prehypertension is therefore, suggestive of impending metabolic syndrome wherein hypertension occurs early rather than than late.
Resting heart rate was significantly elevated among prehypertensives. High sympathetic tone indicated by raised resting heart rate, contributes to worsening of risks relating blood pressure, glucose metabolism and plasma lipids [38]. Resting heart rate monitoring has long term prognostication value among hypertensive [12,39]. In the present study elevated resting heart rate in prehypertensives is not found associated with worsened blood sugar and lipid profiles. It may simply indicate too early stage of the disorder [40].
Homocystein is formed from dietary amino acid methionine and plays pivotal role in folate metabolism and methyl group transfer. Its concentrations are influenced by genetic and environmental factors, especially vitamins folate, B12, B6 as well as certain lifestyle factors and medications. Significance of homocystein as a cardiovascular risk factor depends on synergistic cardiovascular risk factors such as, nutrition and genetic polymorphisms.
Homocystein plasma levels are shown to directly relate to BMI in boys [41]. Metabolic syndrome with hypertension generally accompanies raised blood homocystein levels that correlate directly to prevalence of cardiovascular complications [42]. Based on studies in adolescents, 90th percentile level of homocystein (found as 8.23micro moles/l), was proposed to be treated as cutoff for hyper-homocysteinaemia [43]. Low HDL- cholesterol was considered to substantiate the cardiovascular risk of hyper-homocysteinaemia. In the present study, homocystein levels were also higher than above proposed cut off 8.23micro moles/l. Atherogenic hyperhomocysteinaemia and dyslipidaemia were not significantly in excess of that in controls, suggesting prehypertension as early stage of metabolic disorder.
Study limitation
The limited study sample drawn from a single admission batch of medical students represents only 18 to 20 year age group that belongs to high socioeconomic class of society. The prevalence of findings is not generallizable beyond such specification even for the purely Indian population sample.
Recommendations for early prevention
There is a graded increase in risk moving from optimal blood pressure (<120/80mm Hg) through normal blood pressure (120-129/80-84mm Hg) to high normal blood pressure (130139/85-89mm Hg), as per Framingham population study [44]. People with higher normal blood pressure levels frequently develop hypertension in a decade or two. Hence the potential risk category of prehypertension was proposed [45]. Around 40% adult population in US was found to be prehypertensive [46]. Group of people at high risk of developing hypertension include those with family history of hypertension, overweight or obese, consuming excess sodium and/or insufficient potassium, alcoholics and with sedentary lifestyle [47].
Screening and detection of prehypertension at early stage should facilitate chances to institute such simple measures of disease prevention and health promotion. Prevention of adult hypertensive disease needs to start early in life by identifying families with history of heart diseases and case detection in youngsters in population. Secondary prevention would include screening for disease progression and taking preventive measures to limit complications. The measures include assessment of other risk factors; weekly monitoring of blood pressure; screening for co-morbidities, as obesity, diabetes, hyperlipidaemia. Short term studies support recommendation of lifestyle modification in such subjects [48,49]. Risk factor modification and behavioral change particularly in diet, physical activity, smoking and drinking cessation are found relevant in hypertension.
The lifestyle modification for primary prevention are similar for prehypertension as for hypertension and include:
A. Engaging in regular aerobic physical activity, at least 30 minutes daily on most days [39,50].
B. Weight loss if overweight/obese to maintain BMI in 18.5 to 24.9kg/m2 [51,52].
C. Consumption of diet rich in fruits and vegetables and low in saturated and total fat [53].
D. Reduction of dietary sodium intake to less than 100mmol or 6gm table salt and adequate intake of potassium(90mmol) daily [48,54].
E. Limiting alcohol consumption if any, to under 60ml of 100-proof whisky per day [55].
Prehypertension in people with cerebrovascular or coronary heart disease qualify for anti hypertensive drug therapy [56]. In this context, baseline systolic blood pressure, diabetes and increased left ventricular mass have been used as predictors of risk score for hypertension development [57]. Early intervention for blood pressure control is associated with eventual better cardiovascular outcomes [58,59].
Conclusion
Family history, obesity, and psychological morbidity had higher association with state of prehypertension. Screening is early age is important to unravel prehypertension and metabolic syndrome, especially in subjects with family history of such disorders. Such subjects can be investigated for risk factors and monitored for disease progression. Timely institution of measures for weight reduction, lifestyle modification, dietetics etc, should avert disease progression and complications.
For more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php
For more Open
Access Journals please click on: https://juniperpublishers.com
To know more about Juniper Publishers please click on: https://juniperpublishers.business.site/



Comments
Post a Comment