Every Little Helps-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Introduction
The National Health Service (NHS) is facing an
unprecedented financial burden. We have to save up to £22 billion over
next five years. Some savings can be obtained by efficient working but
the majority can be achieved by working ‘smartly’ and reducing wastage.
Our advances in medicine are putting greater pressure on our finances
and therefore we need to be more focussed to ensure that the precious
resources of the NHS are utilised as effectively as possible.
A large proportion of expenditure found in surgery is
in the theatre environment [1]. Although implants, suture materials and
cardiopulmonary bypass machine are the primary contributors to cardiac
surgery costs, standardization of the surgical process provides an
opportunity to decrease waste and improve efficiency. Cardiac surgeons
can focus on the usage of instruments in theatre and assess the
implementation of cost-effective measures to utilise the resources
effectively. Several authors reported that across four different
surgical specialties, the number of surgical instruments used per case
ranged from 13-25% of the instruments contained on a surgical tray
[2-4].
We found that a large proportion of instruments used
in the cardiac surgery tray are consistently unused. Revising surgical
trays with fewer instruments can result in significant cost savings [5].
The number of instruments on the surgical tray can be reduced by
methodically investigating the requirements of individual instrument
without compromising the fundamental principles of surgery or
conflicting the surgeon’s individual preference. The objective of the
study was to identify the usage of instruments in common cardiac
surgical tray and time utilised by the team in associated with
processing unused instruments.
An observation study was conducted on surgical
instruments in coronary artery bypass graft (CABG) trays. Data was
collected from CABG operations over a period of four months. Four
consultants in the unit were included in the study. Four caseswere
observed in total from each consultant’s theatre lists. The time was
calculated to count the instruments by the scrub nurse. It was repeated
three times for different grades of nurses.
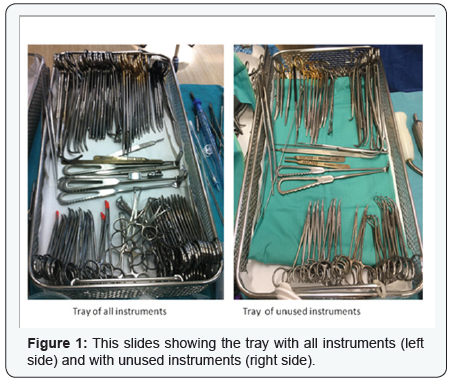
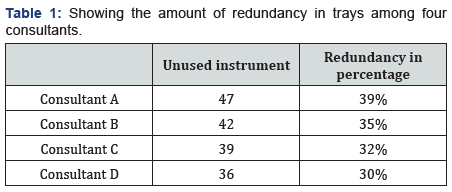
A coronary artery bypass graft tray contains 119
instruments (Figure 1). Forty seven instruments were unused by one
consultant at the end of the procedure. The table shows the individual
consultants’ usage of the instruments (Table 1).
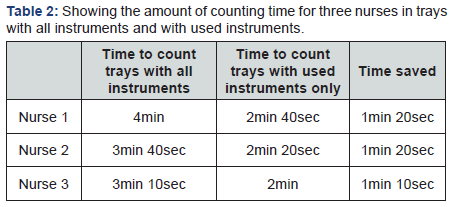
It took three to four minutes by the scrub nurse to
calculate all instruments in the tray. After removing the unused
instruments, the time was reduced to 2mins. It is worthwhile to mention
that the scrub nurses count the number of instruments in every case
three times (Table 2).
From our experience, we found that instruments are rarely
removed from the trays. More often instruments are added to
the trays and that trays have become heavier over the years.
One of the trays weighed approximately 6.4kg. After removal of
redundant instruments, the weight was reduced to 5.2kg. Heavy
trays, and the physical consequences of handling these trays may
contribute to an increase in the dropout rate of employees.
Florijn EP [3] studied a dataset of 12 tray types in the
Academic Medical Centre (AMC) in Amsterdam, and found that on
average 21% of the instruments in the dataset were obsolete. In
our study, overall utilisation of the tray was low with substantial
redundancy ranges from 30-39%. Another consequence of
sterilizing unused instruments is the deterioration of the quality
of material. This leads to a shorter life of the instruments and
quicker replacement of instruments, resulting in higher costs.
Less utilised instruments can be identified and replaced by a
process of individual packing to meet surgeon specific needs.
Single instrument packing can be employed for infrequently
used instruments with a shelf life of 96 weeks. It will reduce
the unnecessary processing of instruments, improve employee
safety and cost effective practice [6]. Removal of redundant
instruments can be ensured by effective input and instruction
from surgeons and scrub nurses. In addition to individual trays,
specific surgical trays (e.g. sternotomy open and closure tray)
could be considered for review in order to eliminate unwanted
instruments with potential savings of time, resources and
cutting wastage.
It is well established that excess time spent counting
instruments significantly compromises case progression in the
theatre [7]. Time savings should be considered from the starting
point of the cleaning, disinfecting and counting of instruments in
the sterilisation unit [7,8]. Furthermore, autoclaving for smaller
trays results in reduced sterilisation time. This improves the
total turnover time of trays. There is reduced chance of missing
instruments when fewer instruments are in the tray. We have to
consider human error in this sterilisation process [9]. Stockert
et al. [10] noted that there was a 49% error rate for trays with
greater than 40 instruments contrasted against an error rate of
13% for trays with 40 instruments or less.
Van Meter et al. [4] have reported that excess processing
cost can be saved by removing unwanted instruments from
surgical tray [5]. We estimated that the cost for sterilisation of
unused instruments per tray is £3.00. Average 17,630 coronary
artery bypass procedure was done in 2013 in UK, we can save
upto17,630 X £3.00 =£52,890 [7]. If we apply similar principle
in all cardiac surgery in 2013, the potential savings could be
36,134X £3.00=£108,402 in 2013 [11].
This simple concept can be applied to all surgical specialities.
Here, we are looking for marginal gain. This small step in waste
reduction and cost saving measures can make a considerable
impact in the theatre management. This humble challenge
should not be underestimated and can be translated into
significant cost savings in the long term.
Data was collected on only one surgical procedure in cardiac
surgery. Usually, instruments are variable in different cases.
The cost of individual packing of single instruments was not
measured and compared with the set of instruments in the tray.
We did not visit the sterilization suit and were not able to count
the time spent to process the instruments over there.
This small study focuses on the advantages of small changes
to reduce the cost and also to promote competency for utilising
limited funding. Further research is warranted to investigate
the efficiency of surgical processes for effective utilisation of
precious resources in NHS.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php
To know more about Juniper Publishers please
click on: https://juniperpublishers.business.site/



Comments
Post a Comment