Eosinophilic Heart Disease: A Case Report and Review of Literature-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Introduction
Hypereosinophilic syndrome (HES) is a multisystem
disorder diagnosed by the presence of hypereosinophilia (HE) defined as
an absolute eosinophil count (AEC) >1.5x109/L (or
>1500cells/microL) and multi organ involvement attributable to HE.
Myocardial dysfunction is a frequent finding and is a major cause of
morbidity and mortality in HES. The diagnosis of hypereosinophilic heart
disease (EHD) is made in the setting of hypereosinophilia and
characteristic clinical features and imaging findings of damage to the
heart. We describe those clinical features in this case of HES with HHD
with review of literature.
A 63 year old male with no known past medical history
was transferred to our hospital for hypotension, abnormal EKG and
elevated troponin. The patient described nonspecific symptoms of cough,
runny nose, malaise, muscle aches, nausea, diarrhea and low grade fever
for 2-3 weeks. He also noted a skin rash which had resolved at the time
of admission. He denied air travel outside the United States, no prior
known malignancies or inflammatory diseases such as vasculitis or
autoimmune diseases. He has no history of diabetes mellitus,
hypertension or hyperlipidemia but is an active smoker. His examination
revealed diminished lung sounds bilaterally, normal heart sounds with a
soft 1/6 intensity holosystolic murmur without marked radiation of the
murmur. There was mild lower extremity edema present. His
electrocardiogram showed sinus rhythm with diffuse T-wave inversions. He
had a contrast enhanced CT of his chest abdomen and pelvis which
revealed no pulmonary embolism or dissection, marked lymphadenopathy and
small pleural effusions only. His pertinent laboratory data revealed
hyponatremia, normal creatinine and an elevated troponin I value of
2.89. He was found to have an elevated white blood cell count of 15000,
hemoglobin 9 gram/dl and platelet count of 40,000. His eosinophil count
was 4800 (UNITS). A transthoracic echocardiogram revealed hyperdynamic
left ventricular (LV) systolic function and apical thickening concerning
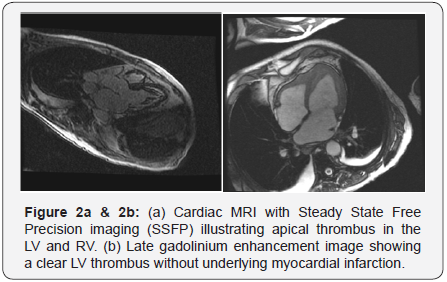
for an LV thrombus (Figure 1a & 1b). An MRI of the heart confirmed
the diagnosis of apical thrombus along with fibrotic material seen in
both LV and RV apex (Figure 2a & 2b). In the presence of
hypereosinophilia and the imaging findings a diagnosis of HES was made.
He was initiated on anticoagulation.

HES are a heterogeneous group of disorders. Typically
symptoms are very nonspecific as in our case. A rash, GI
disturbances, cough and dyspnea are the common symptoms.
Myocardial involvement in HES was first described in 1936
by Wilhelm Loffler who reported a ‘fibroplastic parietal
endocarditis with blood eosinophilia’ [1]. Prevalence of EHD
in HES is up to 50% [2,3]. Myocardial dysfunction is a major
cause of morbidity and mortality. Hence timely diagnosis and
treatment may improve patient outcome [3,4].
Pathophysiology of EHD includes three overlapping stages:
1) an acute necrosis, 2) thrombosis and 3) fibrosis. Acute necrosis
is felt to be caused by eosinophilic infiltration and activation
with release of inflammatory mediators and toxic proteins. In
second stage, at the site of damaged and exposed endocardium,
platelets bind with von Willebrand factor and collagen to form
a thrombus. Thrombus formation can occur in both ventricles
typically at the apices. However, it can be located at the valvular,
subvalvular or in the outflow tracts. Systemic thromboembolism
remains a major concern of morbidity and mortality in up to
25% of patients. In the final stage, thrombosed endocardium is
replaced by fibrosis resulting in scarring, valvular regurgitation
and restrictive cardiomyopathy. The clinical presentation of EHD
is variable and may range from an asymptomatic myocardial
involvement to heart failure syndrome, conduction abnormality,
fatal arrhythmia, sudden cardiac death or an acute coronary like
syndrome. Arrhythmias are due to fibrosis of the conduction
system or myocardial scarring. Acute coronary syndrome is rare
but can occur due to embolic coronary artery occlusion [5-7].
It is important to note that EHD can be seen in any cause
of eosinophilia or hypereosinophilia such as drugs and
hypersensitivity reactions, parasitic or protozoal infections,
malignancies or idiopathic hypereosinophilic syndromes [8].
Medications are frequently implicated as an etiology of
hypereosinophilia. A wide spectrum of drugs can lead to HE
and include antimicrobials, anti-inflammatory, antipsychotics,
anticonvulsants, diuretics, inotropes and ACE inhibitors
[9,10]. Eosinophilic myocarditis has also been described
with hypereosinophilic vasculitides such as eosinophilicgranulomatosis with polyangiitis (EGPA). HE can be reactive
or part of a proliferative clone in solid and hematological
malignancies such as lung, GIT, urogential tumors, T and B
cell lymphomas, acute and chronic myeloid leukemia and
myeloproliferative disorders.
Endomyocardial biopsy is the reference standard test for
the definite diagnosis of EHD. However, biopsy is often not
performed due to its invasive nature, leaving the diagnosis made
based on the appropriate clinical data and imaging modalities.
It is important to note that a biopsy may be negative in cases
with focal cardiac involvement. Eosinophilia is present in the
majority of the patients with EHD. Electrocardiographic changes
are common but nonspecific and may include criteria for left
ventricular hypertrophy, arrhythmias, first degree AV block.
T-wave inversions are most frequently found as seen in our case.
T-Wave inversions are likely manifestations of subendocardial
injury and fibrosis [11]. Echocardiography plays a vital role in
suspecting and identifying EHD. Echocardiographic findings may
vary depending on stage of presentation and degree of myocardial
involvement. Characteristic echocardiographic features of EHD
include endomyocardial thickening in up to 68% of the cases,
apical obliteration/thickening due to thrombus formation and
restricted posterior mitral leaflet. Other conditions such as
LV noncompaction, apical hypertrophic cardiomyopathy and
isolated LV apical thrombus may mimic the echocardiographic
images of EHD. Different imaging techniques such as use of echo
contrast agents, transesophageal echocardiography with three
dimension windows and magnetic resonance imaging (MRI)
can make the differentiation among these conditions [11-13].
In fulminant cases of myocarditis, a non-dilated, thickened,
and hypocontractile left ventricle (LV) is usually observed.
Myocardial fibrosis can result in restrictive cardiomyopathy in
later stages which can be assessed with Doppler data. Cardiac
MRI has higher sensitivity and specificity than any other
imaging modalities and contrast-enhanced Cardiac MRI can
identify inflammation and fibrosis in its early stages even when
echocardiography findings may be normal [14-17]. Interestingly,
the severity of eosinophilia was directly related with the severity
of MRI findings in few case reports [17]. In our patient, Cardiac
MRI showed circumferential apical endocardial thickening/
fibrosis after gadolinium contrast administration and LV apical
thrombus, which is pathognomonic of EHD. Cardiac computed
tomography (CT) may be used to evaluate the coronary artery
disease as a potential cause of apical thrombus if concomitant
wall motion or severe systolic dysfunction is present [18].
Coronary angiography has little role and is only used to rule out
coronary artery disease.
Treatment of EM involves both pharmacologic and nonpharmacologic
therapies. Pharmacologic therapies include
guideline driven therapies specific to cardiac presentation,
anticoagulation and steroids. In addition it is important to find
the etiology of hypereosinophila and treat it accordingly. Insuspected cases of drug hypersensitivities, offending drug needs
to be discontinued and chemotherapeutic agent is used for solid
and hematologic malignancies. Patients with Churg Strauss
syndrome are treated with steroids with or without steroid
sparing agents. Recently non FDA approved therapeutic agents
targeting IL-5 receptors as Benralizumab have shown promising
reduction in blood and tissue eosinophilia [19].
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on: https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment