Clopidogrel Induced Thrombotic Thrombocytopenic Purpura-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Clopidogrel is commonly used drug in cardiology
practice. Though apparently benign, it can rarely caus! e Thombotic
Thrombocytopenic Purpura (TTP). Mechanism of action by which Clopidogrel
causes TTP is different than usual. This makes the situation more
interesting. Here we are presenting a case of NSTEMI who developed TTP
after Clopidogrel. Diagnosis is purely clinical. Early diagnosis and
plasmapheresis is lifesaving. A 66-year-old female presents to the
hospital for new onset of chest pain. After laboratory and diagnostic
workup, NSTEMI was diagnosed. Patient underwent catheterization where
triple vessel disease was found, only amenable to CABG. During treatment
of NSTEMI, patient received Clopidogrel for 2 days, which was
subsequently held in preparation for CABG. After CABG, Clopidogrel was
restarted and patient started having dramatic decreases in platelet
count and haemoglobin requiring blood transfusions. Peripheral smear
showed schistiocytes,polychromasia , nucleated red blood cells and low
platelets. Because of persistent platelet drop, haemolysis and uraemia
concern for TTP was raised. As Clopidogrel was recently started, it was
considered the etiological factor. Clopidogrel was held, and plasma
exchange was immediately started with steroid therapy while ADAMSTS-13
levels were pending. After 7 days of plasma exchange and 5 days of
steroids, platelet counts and haemoglobin subseq! uently increased to
appropriate levels. ADMASTS-13 levels came back normal indicating
different mechanism to induce TTP than what has been widely studied in
the literature.
Patient Case
A 66 year-old-female with past medical history of
chronic kidney disease stage 5 (CKD-5) not on hemodialysis,
hypertension, diabetes mellitus type 2 presents to the emergency
department with new onset chest pain and shortness of breath for the
past two weeks. Vitals revealed patient to be saturating 86% on room
air, requiring 3L of nasal cannula. All other vitals stable. On physical
exam, patient had a jugular venous distention. Bilateral course rhonchi
were heard on pulmonary exam. All other physical exam findings were
normal. Laboratory results revealed hemoglobin of 8.9, which was
patient’s baseline, platelet count of 266, creatinine of 6.2. Patient
had a troponin elevation and T wave inversion in lateral leads. Due to
concern for NSTEMI, patient was given Aspirin 325mg and Clopidogrel 75mg
and taken for left heart catheterization the next day.
Patient, on day of catheterization was given 300mg of
Plavix. Catheterization revealed triple vessel disease, amenable to
CABG. Plavix was held for 9 days as patient was awaiting platelet
function to improve for CABG. During the interim, patient had worsening
renal function secondary to contrast load during catheterization, and
hemodialysis was started. Patient was also requiring packed red blood
cell transfusions for hemoglobin of 7. EPO was also started because of
low iron and TIBC levels secondary to chronic disease from CKD. CABG was
performed on day 10 of hospital stay. Patient tolerated surgery well
and clopidogrel was restarted after surgery was performed.
The evening of CABG, patient had a significant
platelet drop to 89 with no signs of bleeding. Patient did start to have
easy bruising of extremities. There was also concern for a concomitant
thrombogenic process secondary to patient’s dialysis line forming clots
twice within a three day period. 4T score was 4. Heparin was held and
Heparine Induced Thrombocytopenia work up was sent. Platelet continued
to drop on Argatroban, which made us to think of another diagnosis as
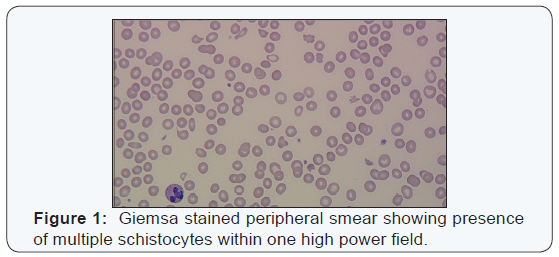
etiology. A peripheral smear was performed which showed numerous
schistocytes. LDH was 572, Reticulocyte count was 4.67, Haptoglobin was
46. Because of thrombocytopenia, hemolytic anemia and worsening kidney
function, TTP was a concerning differential diagnosis, especially
after recent administration of clopidogrel.
Clopidogrel was immediately held and patient was started
on plasma exchange therapy as ADAMST-13 was pending.
Prednisone 80mg daily was started as well. Mean time HIT
antibody came back positive but Serotonin Release Assay was
negative. Platelet count went up subsequently in the next few
days with Plasma exchange with after 7 days of plasma exchange
therapy and 5 days of prednisone therapy, platelet count went to
122 and hemoglobin 9.5 without any need to additional blood
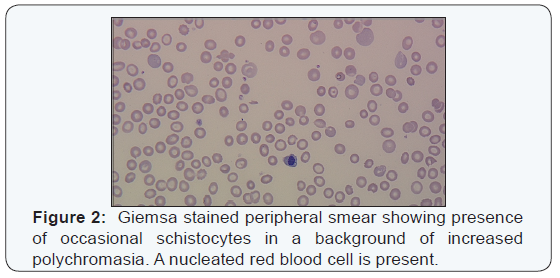
transfusions. Peripheral smear revealed decreased schistocytes
and increased platelets. ADAMTS-13 was found to be normal.
TTP is known as a thrombotic microngiopathic syndrome,
which can be caused acquired or hereditary etiology. The
acquired form, as seen in this patient, is caused by auto
antibodies that form against the metalloprotease ADAMTS-13
[1], which ultimately cleaves von-willibrand factor, a large
multimer. A decrease in this protease activity allows this
large multimer to bind to platelets and in turn, creating
microthrombi, thrombocytopenia and microvascular occlusion
[2]. Microangiopathic hemolytic anemia (MAHA) is also seen
in the form of schistocytes as erythrocytes are damaged by the
large multimer-platelet complexes. TTP classically includes
a pentad of features: MAHA, thrombocytopenia, fever, renal
abnormalities and neurologic disturbance [3]. In this case, the
TTP was medication induced secondary to clopidogrel usage.
According to the Oklahoma TTP-HUS registry in 2013, in the
adult population, TTP is seen in 3 cases per one million adults,
76% of whom were females [4].
Clopidogrel is an anti-platelet medication commonly used
in conjunction with aspirin mainly for patients during acute
coronary syndrome or after percutaneous coronary intervention
(PCI) to prevent re-instant thrombosis. The medication works by
irreversibly blocking the P2Y12 component of the ADP receptors
on the platelet surface, which ultimately prevents platelet
aggregation [5]. Clopidogrel has widely replaced Ticlodipine,
another structurally similar antiplatelet medication, due to its
larger safety profile [6]. Ticlodipine was found to have elevated
incidences of TTP, about 1 in 1600 patients treated. In contrast,
clopidogrel induced TTP has only been noted in a few case
reports [7]. It has been reported by a pharmaceutical supplier
that the rate of clopidogrel induced TTP is about 12 in 1 million
patients receiving the medication [8].
The mechanism of action in clopidogrel induced TTP differs
from what is normally seen. In contrast to low ADAMTS-13
secondary to an autoantibody reaction, there is normal protease
activity in cases where clopidogrel is involved, as seen in our
patient [9]. A study by Bennet et al exploring the different
mechanism of thienopyridine associated TTP, 75% of patients
that received clopidogrel are found to have an ADAMTS-13 level>15% at the time of diagnosis of TTP. The exact mechanism
by which clopidogrel induces TTP has not been well studied.
A theory of endothelial cell wall damage has been introduced.
Because of normal levels of ADAMTS-13, endothelial cell wall
damage allows the secretion of these large multimers of VWF,
which have been studied in mouse models, inducing TTP [7].
The timeline for clopidogrel induced TTP also differs from
other medication induced TTP’s. Signs of TTP are seen within
a 2 week of receiving clopidogrel, which is in contrast to other
thienopyridines in which TTP occurred within 2-12 weeks of
medication administration [10]. This patient started presenting
with TTP about 9 days after clopidogrel administration. This
also strengthens the notion that patients diagnosed with TTP
within a short amount cannot allow for auto antibodies to form
against ADAMSTS-13, allowing another mechanism to cause
TTP. Because of normal ADAMTS-13 levels, the diagnosis of TTP
is primarily clinically based on symptomology and lab values
(Figures 1 & 2).
Treatment for TTP should be started as soon as possibly
secondary to the high mortality associated with TTP. Because
clopidogrel induced TTP is very rare, management is mainly
based on case reports and that of routine treatment for TTP.
Clopidogrel should be immediately discontinued and plasma
exchange therapy should be considered immediately. Survival
amongst patients who received TTP was about 70% for those
patients who received plasma exchange [9]. Plasma exchange
therapy should continue until platelet count is over 150 thousand
for at least 3 days. High dose steroids should also be started at
the time of diagnosis and tapered once patient has a platelet
count that has plateau to acceptable levels [9]. Our patient has
received 7 cycles of plasma exchange therapy with improvement
in platelet count to above 150 after day 4. Our case demonstrates the different mechanism that clopidogrel undergoes to cause
TTP then what has widely been studied.
For more articles in Open Access Journal of Cardiology & Cardiovascular
Therapy please
click on:
https://juniperpublishers.com/jocct/index.php
https://juniperpublishers.com/jocct/index.php



Comments
Post a Comment