Transcatheter Membranous Ventricular Septal Defect Closure, with Nit-Occlud PFM Device in One Working Group, Long-Term Follow up-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS JOURNAL OF CARDIOLOGY & CARDIOVASCULAR THERAPY
Abstract
Objective: Goal of this work was
to evaluate the safety and efficacy of transcatheter closure of
ventricular septal defect (VSD) perimembranous (pVSD) with pfm device,
Nit - Occlud, and long-term results. The VSD is the most common
congenital heart disease being mostly membranous. Transcatheter
percutaneous closure is a novel technique.
Material and methods: Between
December 2004 and December 2013, 300 patients with VSD record were
admitted to our study, previously admitted to the cath lab at our center
for percutaneous treatment of its VSD with different types of devices.
All patients were followed until December 2013, between 1 and 109
months. Cases closed with Devices pfm, Nit Occlud is therefore selected.
There was thus obtained a sample of 59 cases, 5 cases were dismissed
for having no full registration and review of 54 cases was performed.
The age range 17 months to 16 years. The VSD type was treated
perimembranous 100%. Sub Aortic 12, Sub tricuspid 27, Basal medium 5,
and membranous muscle 5, not specified 5. pVSD aneurysm 51, 94.44%. VSD
measures were between 1.5 and 16 mm, made by echocardiography or
ventriculography. The successful placement of the device was 92.59%. The
type of device used was Nit Occlud Coil VSD Le 35 cases, 64.81%, Nit
Occlud PDA 19 cases, 35.18%. Complications were mostly minor; among the
most relevant major complications was transitory hemolysis in 2 cases,
4%. There were no complete AV blocks between them.
Conclusion: Percutaneous closure
of perimembranous VSD in experienced hands with Nit Occlud device of
pfm can be performed safely and successfully with low morbidity and
mortality. Long-term results are favorable, with the percutaneous
closure of perimembranous VSD is a less invasive alternative and could
be taken as first choice in the treatment of membranous ventricular
septal defects.
Abbreviations: VSD: Ventricular
Septal Defect; PVSD: Perimembranous Ventricular Septal Defect; MVSD:
Muscular Ventricular Septal Defect; CAVB: Complete Atrio-Ventricular
Blockade; QW: Quick Way; LV: Left Ventricule; RV: Right Ventricule; RS:
Residual Shunt
Introduction
Introduction
The Ventricular Septal Defect (VSD) is the most
common congenital heart defect, and its variant perimembranous
(perimembranous VSD) are the highest percentage of them, 70% [1-5].
Percutaneous closure of VSD is only approved in the literature for
Muscular VSD (MVSD) [6-9], since in the perimembranous VSD Standard
treatment is surgery with extracorporeal circulation [10-29] due to the
high rate of complications reported in percutaneous procedures such as
complete atrioventricular blockade (CAVB) [30]. Yet the Standard
Surgical treatment has risks as CAVB 1.1%, Post Pericardectomy syndrome,
residual shunts, besides being a more invasive method for the patient
[10,17,29].
Cardiac Catheterization is an alternative to the VSD
closure, tested as a method of first choice in closing muscle VSD [6-9]
and exists as an alternative treatment in perimembranous VSD since the
first reports of percutaneous VSD closure in 1988 [30-56]. This work
demonstrates that the percutaneous method
is a successful and low morbidity and mortality alternative
in the procedure as well as in long-term Follow up of the VSD
closure and specifically perimembranous VSD . In this paper
perimembranous VSD closure with Nit Occlud device Coil
reported. This work is a single working group with long-term
follow up.
Materials and Method
Materials and Method
Material
It was taken for analysis record of all patients diagnosed
with VSD by the working group Hemodynamics Laboratory
of Cardiology at Children’s Hospital J.M. Los Rios, Caracas,
Venezuela, between December 2004 and December 2013 in
a sample of 300 cases treated in the cath lab 59 cases treated
with Coil Nit Occlud of pfm was selected, discarding 5 cases for
not having complete records and 54 cases of membranous VSD
closure with pfm Nit Occlud coil were processed.
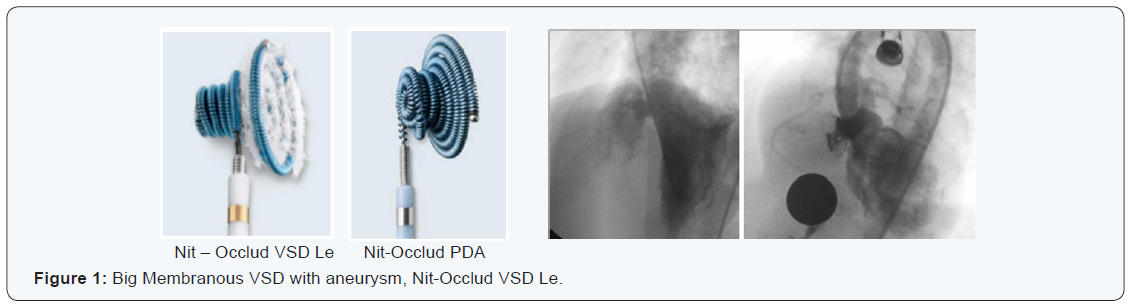
Devices: The devices used were Nit - Occlud Brand , Spiral
Coil Sistem, pfm house : NIT- Occlud VSD Le, NIT- Occluded PDA.
Method
All features of the technique, patients and pathology
described , namely: Access Road: 2 options, the Retrograde,
Quick Way (QW ) in which the catheter is passed from Left
Ventricule (LV) to Right Ventricule (RV), the device first cone
is deployed in the RV and then the second cone is displayed in the LV. Loop method in which the VSD is passed from the left
ventricle is advanced with the right guide to a cavity as vena cava
or pulmonary artery, the guide is captured and exposed outside
the patient by establishing a Femoral Artery -vein loop, the
transport catheter of the device progresses from the vein into the
left cavities to the Aorta, specifically with Nit - Occluded Spiral
Sistem, the device first cone is exposed in the Aorta, deployed at
LV and then the second cone is displayed in the RV.
Patients studied and their characteristics: Total patients
(p) with VSD, 54.
4.2.2 Gender: Female Dominance 57.4%.
4.2.3 Age: Between 17 months and 16 years.
4.2.4 Weight: Between 8 and 53 kg.
VSD type: Described in 54p, 54 Membranous, 100% (Table
1).
Symptoms such as fatigue, weight gain difficulty; medication
used for heart failure; Echocardiographic findings: Qp/Qs ratio,
AI/Ao ratio, radiological findings: Cardiomegaly, hyperflow or
venous congestion. Assigning one point to each for a total of 5
[1-5,57,58].
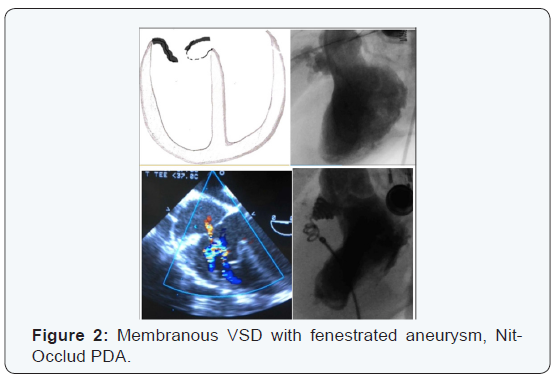
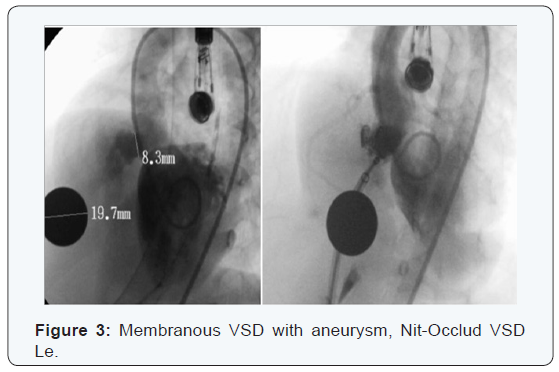
VSD size: Measured by Trans- Thoracic Echocardiography,
transesophageal echocardiography or catheterization. Range of
1.5 to 16 mm (Figures 1-3) (Tables 2-4).
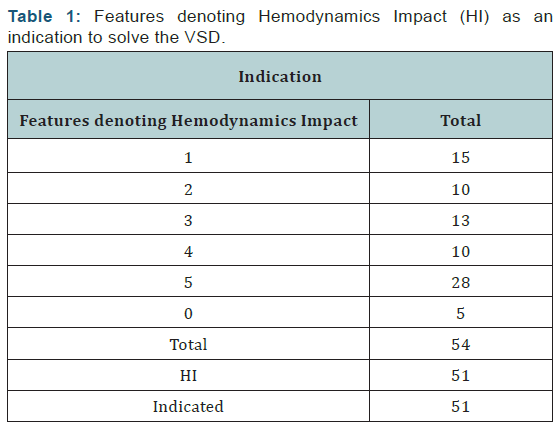
The percentage of patients with indication was 94.44 %.
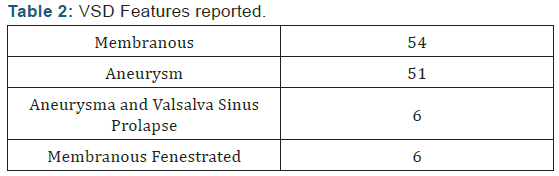
Membranous features: Described 54p, Aneurysm (Aneu) 51 p, 94.44
%;
Fenestrated 6p, 11.11 %; with Valsalva Sinus Prolapse (VSP) and
Aneurysm 16p, 11.11 %.
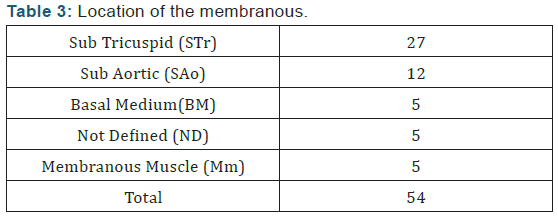
Location of the membranous: Described 54p, 100% STr 27p, 50%;
SAo 12p, 22.22%; 5p BM

Concomitant diseases, congenital heart disease or Acquired type
Total 9p, 17 %; 2 cases with PFO closed in the same
procedure with Amplatzer PFO; 1 patient with Mild Pulmonary
Stenosis dilated with balloon in the same procedure; 1 case with
ASD ; 1 Case with ASD and PDA which failled closure the ASD
with Hellex and failled Closure PDA with Nit Occlud PDA; 1 VSD
previously closed with Nit Occlud VSD Le and residual VSD a new device Nit Occlud VSD Le was implanted; 1 VSD Closed Surgically
with Residual VSD was closed with Nit Occlud VSD Le, 1 Case
had been previously tried to close with Amplatzer and made a
transient complete AV block so the catheterization was aborted,
was closed with Nit Occlud VSD Le; 1 case with Mitral Stenosis
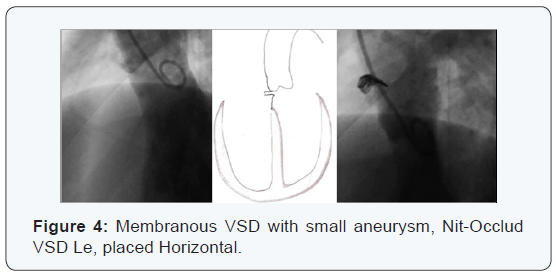
and Mitral parachute (Figure 4).
Results
Procedure time
Heparin time was measured, Heparin was placed once VSD
diagnosed by TEE or Catheterization, and was counted until the
VSD was closed; and fluoroscopy time. Heparin average time was
36 minutes; fluoroscopy average time was 30 minutes.
Access Road
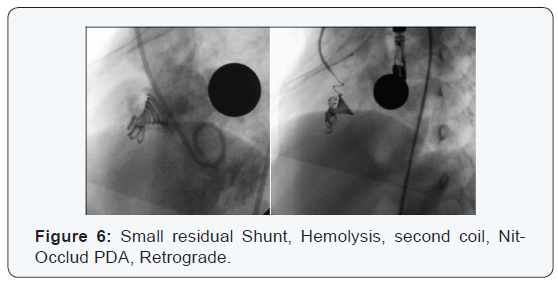
Only one case was closed Retrograde Quick Way from VI,
residual restrictive VSD case presented Hemolysis and placed a
PDA Nit Occlud to stop hemolysis (Figures 5 & 6).

Success of the procedure
It was considered:
- Succeeded: all VSD Closed
- Failed: all attempts to close VSD, crossing the VSD with the catheter without achieving close it
- Aborted: VSD that for some reason or feature is not trying to cross the VSD with the catheter.
- Successful: 50 cases, 92.59%;
- Failed: 3 cases, 5.55%;
- Aborted: 1 Case, 1.85%.
If we take into account the premise of not closing those
present TCAVB in the procedure, the success rate is 94.33 %, 50
cases of 53 procedures.
The causes of failure were: 1 case migration to VD, being
rescued; 1 case the device is jam when passing through the
aortic valve, when achieve release it migrated to VD; 1 patient
with ASD, PDA and VSD already closed with Nit Occlud VSD Le
in the same procedure, in the process trying to close the PDA the
device is hooked already placed migrating, being rescued later,
the ASD was unsuccessfully tried to close with Hellex. The cause
of Aborted: 1 case for transient AVB.
The results according to the characteristics of the VSD was assessed by type: Ratio VSD Size and Device size
The Nit - Occlud is recommended to oversize the bigger loop
2-4 mm relative to the opening of the VSD, ie , we take equal size
to that dimension of the Loop least 4. Fulfilled with the approach
of not overstate the device to seek to avoid the complication of
permanent AVB to cause pacemaker, as also in some cases smaller
devices were used to leave the device inside the aneurysm [48].
2nd device placed in the same patient: 2p, of 50 closed,
3.70%; ie, 1p Nit -Occlud VSD Le with Hemolysis solve placing
the 2nd Coil Nit - Occlud PDA in the first week, (reported in
hemolysis ). We report a late second case 1p perimembranous
VSD STR withaneurysm of 10mm, closed with NIT-Occlud VSD
Le 10x6, migrated into the aneurysm, with rsidual shunt for
3 years, was placed on the 2nd Nit VSD Le 12x6, stays with
minimum residual shunt with minimum Hemodynamics Impact,
then the 1st device found migrated and healed in right branch
of the pulmonary artery, was attempted to remove it and failed
(Figures 5 & 6).
Follow-up time: Between 1 month and 109 months.
Complications: Immediate
Residual shunt (RS)
Immediate in the catheterization, 20p of the 50p with
device 40 %; of them 12p with Nit-Occlud VSD Le, 8p Nit-Occlud
PDA,(This device is not designed for VSD closure and is not a fiber-
Coil). At follow-up: still wit RS at 24 hour follow-up 11p 22%, all
with VSD Le Nit Occlud. All Nit-Occlud PDA Shunt disappeared
in 24 hours. Subsequently the RS disappeared one month 7p,
14 %; 5p more disappear on their follow-up to 2 months 2p,1p to 1 year, 2 years and 5 years respectively. Subtracting 2p
4% of the Nit-Occlud placed persists with minimal RS without
Hemodynamics Impact at 9 years of follow up.
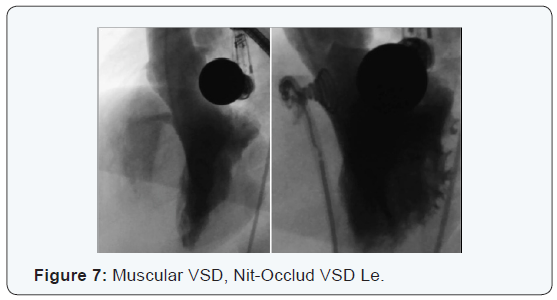
Transient hemolysis
Starts in the first hours after catheterization, 2p of the 50
closed, 4%. 1p Nit-Occlud PDA of the 19p with Nit- Occlud PDA,
5.26 %, is spontaneously resolves the 2nd day, this tipe of device
is no designed to VSD closure, hemolysis subsides spontaneously
within 2 days. 1p Nit -Occlud VSD Le of the 35p with that tipe of
device, 2.85 % with RS and hemolysis was placed a 2nd Coil Nit
Occlud PDA quick Way a week latter and the RS and hemolysis
disappeared in 5 days [52] (Figures 5-7).
Immediate Migration: Total 3p of the 54p, 5.55 %. They are
rescued named in failed cases.
Migration remaining within the aneurysm: 2p migrated
into the aneurysm, 4%, namely: 1p Nit-Occlud VSD Le migrated
into the aneurysm (named in placing 2nd device on the same
patient in long-term follow up); 1p with Nit-Occlud VSD Le
migrating into the aneurysm with RS, removed in surgery at 7
years (named in Surgery).
No Progress transport pod RV to LV throught the VSD: 1p
solved with Nit - Occlud PDA ASA Way, because the transport pod
is 5F (Figure 2).
Migration in the follow up: 1p of the 50 placed 2%; NIT
VSD Le migrated to 7 years (reported in 2nd placement device).
Rhythm disorders Transient immediately or in the
follow up: 1 transient 1st grade AVB disappears immediately.
1 Transient right bundle branch Block disappears immediately.
Permanet Branch Block in the follow up: 1p of the 50
closed, 2 %; Hemiblock of the anterior subdivision of the left
bundle branch Hiss in the follow up without Hemodynamics
Impact, VSD STR aneurysm, Nit-Occlud VSD Le [51].
Surgery in the follow up: 1p, 2%. Nit-Occlud VSD Le
migrates into the aneurysm, persisted with RS, at 4 of year
follow-up showed thrombocytopenia classified as Marrow
Aplasia meriting bone marrow transplant, thrombocytopenia
persisted until the removal of the device and close the VSD for
large RS to 7 years [31,59].
Discussion
Discussion
High level of success in closing perimembranous VSD with
Coil Nit Occlud. There were no CAVB including the following
9 years. Most complications were transient, 2p with residual
shunting without hemodynamic impact to 9 years and only by
large RS 1P and thrombocytopenia removed in surgery at age 7,
2% on follow up to 9 years [60-65].
Conclusion
Transcatheter closure of aneurysm perimembranous VSD
with Nit Occlud Coil device has high chance of success with a low
level of complications.
For more articles in Open Access Journal of
Cardiology & Cardiovascular Therapy please click on:
https://juniperpublishers.com/jocct/index.php
https://juniperpublishers.com/jocct/index.php


Many Efforts to explain the crucial information
ReplyDeleteTranscatheter Valve Consulting
Bovine Pericardium Tissue